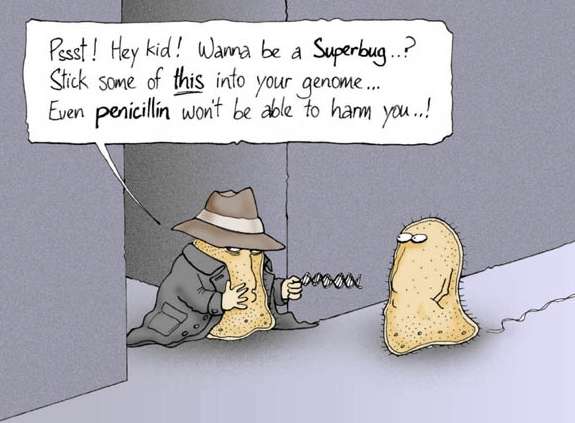
FDA Approved Antibiotics which are marketed internationally. The
problem of the antibiotic resistance has been over-viewed in the previous article. Here are the latest antibiotics in current use.
Oxazolidinones
In clinical use: Linezolid In clinical trials: Radezolid, torezolid.
Effective against Organisms-
–gram-positive bacteria including MRSA, VRE and Streptococcus pneumoniae.
–Mycobacterium tuberculosis and Nocardia.
Linezolid- 1st to be approved this millenium
Indicated-
–VRE infections
–nosocomial and community-acquired pneumonia,
–skin and soft tissue infections.(SSTIs)
Bacteriostatic against drug-resistant organisms like MRSA and VRE. Inhibits bacterial protein synthesis at an early stage and inhibits the formation of a functional initiation complex.
Resistance- Mutations in the peptidyl transferase centre of the rRNA
Serious adverse effects – bone marrow suppression, peripheral and optic neuropathy, lactic acidosis, and serotonin syndrome.
Clinical Outcomes of Linezolid vs Vancomycin in Methicillin-ResistantStaphylococcus aureus Ventilator-Associated Pneumonia -Retrospective Analysis Jeannie D. Chan Et Al
Vancomycin has been the treatment standard for methicillin-resistantStaphylococcus aureus (MRSA) infections, but clinical efficacy is limited.
A Retrospective analysis of 113 participants with MRSA VAP confirmed by bronchoscopy who have been initiated on therapy with either vancomycin or linezolid within 24 hours after bronchoscopy and completed ≥7 days of therapy during their hospitalization from July 2003 to June 2007. The primary endpoints were hospital survival and clinical cure, defined as resolution of signs and symptoms of VAP or microbiological eradication after completion of therapy along with clinical pulmonary infection score (CPIS) ≤6 at day 7 of therapy.
Results: At hospital discharge, 23/27 (85.2%) of linezolid and 72/86 (83.7%) of vancomycin recipients had survived (P = .672). In comparison to linezolid recipients, the adjusted odds ratio (OR) for survival was 0.72 (95% confidence interval [CI]: 0.16-3.27) with vancomycin therapy. Clinical cure was achieved in 24/27 (88.9%) of linezolid and 63/86 (73.3%) of vancomycin recipients (P = .066).
Compared to linezolid recipients, the adjusted OR for clinical cure was 0.24 (95% CI: 0.05-1.10) with vancomycin therapy. Survival and clinical cure did not differ significantly between vancomycin recipients with trough level ≥15 and <15 μg/mL, respectively.
Conclusions: No survival benefit but a trend toward higher cure rate with linezolid therapy. J Intensive Care MedNovember/December 2011 vol. 26no. 6 385-391
ZEPHyR study
The ZEPHyR (Linezolid in the treatment of subjects with nosocomial pneumonia proven to be due to methicillin-resistantStaphylococcus aureus) study was the largest ever conducted in this population. Investigators from 156 centers worldwide randomized 1,225 patients, of whom 448 patients had proven MRSA nosocomial pneumonia (modified intent-totreat group); 339 patients also met key protocol criteria at the end of study (per-protocol group) and were included in the primary analysis.
In the per protocol group, 125 patients treated with linezolid (68.3%) and 140 (74.5%) treated with vancomycin were ventilated at baseline
Clinical success rates at the end of study were 57.6 percent (95/165) for patients treated with linezolid compared with 46.6 percent (81/174) for patients treated with vancomycin in the per-protocol group, the primary endpoint. These results demonstrated that linezolid achieved a statistically significantly higher clinical success rate compared to vancomycin (95% CI for the difference in response rates: 0.5%, 21.6%; p = 0.042).
Overall mortality was 15.7% for linezolid and 17.0% for vancomycin.
Thrombocytopenia (linezolid 1.3%, vancomycin 2.2%) and renal failure (linezolid 3.8%; vancomycin 7.2%) occurred at relatively low rates.
Walkey et al combined 8 randomized trials including 1,641 people with MRSA pneumonia, and found no significant differences between those treated with linezolid or vancomycin in survival, resolution of clinical pneumonia, eradication from sputum of MRSA, or adverse events. Authors dispute linezolid’s supposedly higher lung penetration, pointing out that that dogma evolved from studies of healthy people; inflamed lungs seem to retain more vancomycin. .CHEST 2011;139:1148-1155.
Linezolid versus Vancomycin in Treatment of Complicated Skin and Soft Tissue Infections John Weigelt1, et al the Linezolid CSSTI Study Group , American Society for Microbiology, doi: 10.1128/AAC.49.6.2260-2266.2005
a randomized, open-label, comparator-controlled, multicenter, multinational study that included patients with suspected or proven MRSA infections that involved substantial areas of skin or deeper soft tissues, such as cellulitis, abscesses, infected ulcers, or burns (<10% of total body surface area).Patients were randomized (1:1) to receive linezolid (600 mg) every 12 h either intravenously (i.v.) or orally or vancomycin (1 g) every 12 h i.v. ]Linezolid outcomes (124/140 patients or 88.6%) were superior to vancomycin outcomes (97/145 patients or 66.9%) at the TOC visit for patients with MRSA infections (P < 0.001).
The results of this study demonstrate that linezolid therapy is well tolerated, equivalent to vancomycin in treating CSSTIs, and superior to vancomycin in the treatment of CSSTIs due to MRSA.
Linezolid versus vancomycin for the treatment of gram-positive bacterial infections: meta-analysis of randomised controlled trials.
Int J Antimicrob Agents. 2010 Jan;35(1):3-12. doi:10.1016/j.ijantimicag.2009.09.013. Epub 2009 Nov 8. Beibei L, Yun C, Mengli C, Nan B, Xuhong Y, Rui W.
Nine RCTs studying 2489 clinically assessed patients were included in the meta-analysis. Overall, there was no difference between linezolid and vancomycin regarding treatment success in clinically assessed patients [odds ratio (OR)=1.22, 95% confidence interval (CI) 0.99-1.50].
Linezolid was more effective than vancomycin in patients with skin and soft-tissue infections (OR=1.40, 95% CI 1.01-1.95). However, there was no difference in treatment success for patients with bacteraemia (OR=0.88, 95% CI 0.49-1.58) or pneumonia (OR=1.16, 95% CI 0.85-1.57).
Linezolid was associated with better eradication rates in all microbiologically assessed patients compared with vancomycin (OR=1.33, 95% CI 1.03-1.71).
However, nephrotoxicity was recorded more commonly in patients receiving vancomycin (OR=0.31, 95% CI 0.13-0.74).
In conclusion, linezolid is as effective as vancomycin in patients with gram-positive infections. There is superior clinical and microbiological outcome with linezolid in complicated skin and soft-tissue infections caused by Staphylococcus aureus.
Glycolipopeptides
In clinical use: Daptomycin, telavancin Under clinical trials: Oritavancin.
Daptomycin- cyclic lipopeptide with a decanoyl side-chain
Approved by the FDA in 2003 for the treatment of complicated SSTIs caused organisms-
–MSSA, MRSA, Streptococcus pyogenes, Streptococcus agalactiae, Streptococcus dysgalactiae and Enterococcus faecalis (vancomycin-susceptible only).
–Rapid bactericidal activity against most gram-positive organisms including multiple-antibiotic resistant strains.
Shows promise in experimental models of endocarditis, meningitis, ventriculitis, and peritonitis, and is currently approved for use in skin and soft-tissue infections. Ther Clin Risk Manag. 2006 June; 2(2): 169–174.Published online 2006 June.PMCID: PMC1661656A review of daptomycin for injection (Cubicin) in the treatment of complicated skin and skin structure infections. Contraindicated in pneumonia.
MOA- Acts by inserting its lipophilic tail in the bacterial cell membrane resulting in rapid membrane depolarization and potassium ion efflux. This is followed by arrest of DNA, RNA and protein synthesis, and finally cell death.
Drug interactions could occur when daptomycin is used with statins and aminoglycosides.
It causes reversible myopathy as one of its side effects.
Glycopeptides
Telavancin- approved in 2009 for CSSTIs caused by gram-positive bacteria including MRSA strains.
In vitro activity against some vancomycin-resistant gram-positive organisms has been observed.
Dual mechanism of action –
– inhibits peptidoglycan chain formation through blockage of both, transpeptidation and transglycosylation during cell wall formation.
–dissipates membrane potential of the bacterial cell membrane causing an increase in permeability.
Adverse effects-
–vomiting, paresthesias, dyspnea, microalbuminemia, taste disturbances and thrombocytopenia.
–Renal function should be monitored before, during and after telavancin therapy.
–Telavancin is not recommended in pregnancy.
Pleuromutilins
•In clinical use: Retapamulin In clinical trials: BC-3781.
Retapamulin
first pleuromutilin that was approved in 2007 for topical use in the treatment of uncomplicated superficial skin infections.
MOA-
inhibiting protein synthesis. Active against mupirocin-resistant strains.
Retapamulin appears to be approximately 1000 times as potent as mupirocin or fusidic acid against Streptococcus pyogenes.
Effective against many common skin pathogens and has low potential for development of bacterial resistance.
Side effects – pruritus and allergic contact dermatitis.
Newer antibacterials belonging to chemical classes in use before the year 2000
Newer antibacterials belonging to chemical classes in use before the year 2000 are described below
Streptogramins
Newer streptogramins are: In clinical trials: NXL 103.The currently licensed agent- dalfopristin-quinupristin (Synercid), which is available in a parenteral formulation.
Spectrum – MRSA, CONS, penicillin-susceptible and penicillin-resistant S. pneumoniae, and vancomycin-resistant E. faecium but not E. faecalis,VISA
There is little information on dalfopristin-quinupristin and linezolid in treatment of CNS infections, and neither agent is approved for pediatric meningitis.
Indication-
–serious infection with VISA and VRE
–Serious infection with MRSA when Vancomycin is not tolerated
Streptogramin antibiotic (quinupristin) active against vancomycin-resistant E. faecium (VRE) and methicillin-resistant S. aureus (MRSA). Not active against E. faecalis.
Adverse events: Pain, edema, or phlebitis at injection site, nausea, diarrhea, arthalgia,myalgia.
Drug interactions: potent inhibitor of CYP 3A4.
Quinolones
The newer quinolones include: In clinical use: Gemifloxacin, besifloxacin
Many of the new fluoroquinolones have anti-pseudomonal activity and additional anti-MRSA activity.
Gemifloxacin
Oral fluoroquinolone approved in 2003 for treatment of acute bacterial exacerbation of chronic bronchitis and mild-to-moderate community-acquired pneumonia.
shows enhanced activity against gram-positive bacteria( Strep, Staph) and atypical pathogens ( Chlamydia pn, mycoplasma, legionella) but less against Pseudomonas than ciprofolxacin. However, it has poor activity against methicillin-resistant strains.
Anaerobic acivity +
high affinity for DNA gyrase and topoisomerase IV. good activity against fluoroquinolone-resistant strains including fluoroquinolone-resistant H. influenzae.
High concentrations are achieved in the respiratory tract after oral administration, making it an ideal drug for the treatment of respiratory tract infections.
No Ped Dosing available.
Besifloxacin – ophthalmic ointment
Gatifloxacin has been banned due to the risk of severe hyperglycemia.
Trovafloxacin has been withdrawn from the market due to risk for hepatotoxicity.
NXL-101 was discontinued in trials due to prolongation of QT interval
Newer beta-lactam antibacterials
The newer beta-lactam antibacterials include:
In clinical use
Cephalosporins: Cefditoren pivoxil, ceftaroline
Carbapenems: Ertapenem and doripenem. Biapenem is approved in some European countries but not in the United States.
Newer beta-lactam antibacterials in clinical use
Cefditoren pivoxil
oral cephalosporin approved by the FDA for clinical use in 2001. 3rd generation oral cephalosporin with good activity against certain respiratory tract pathogens
Spectrum- S. pneumoniae, H. influenzae and M. catarrhalis, including some β-lactamase producing strains, Staphylococcus aureus (but not MRSA strains) and Streptococcus pyogenes (penicillin-susceptible strains only).
Used in the treatment of mild-to-moderate acute bacterial exacerbation of chronic bronchitis and community-acquired pneumonia, pharyngitis or tonsillitis, and uncomplicated skin and skin-structure infections.
Pediatric use- approved
Ceftaroline and ceftobiprole- ‘fifth-generation’ cephalosporin.
Ceftaroline-
Newest cephalosporin with anti-MRSA activity that obtained FDA approval in October 2010.
Indication-
– acute bacterial skin and skin-structure infections, and
– community-acquired bacterial pneumonia.
Spectrum-
–MSSA as well as MRSA, Strep. Pyogenes, agalactiae, and pneumoniae, hVISA and VRSA
–Gram-negative -ceftazidime-susceptible E. coli and Kleb. pneumoniae, and β-lactamase-positive and negative Haemophilus influenzae,
Synergistic when combined with amikacin, tazobactam, meropenem and aztreonam.
the low potential for resistance development and the favorable safety and tolerability profile in clinical trials, Available IV
CARBAPENEMS-
Ertapenem
1-β-methyl carbapenem approved for use by the FDA in the year 2001.
Spectrum- gram-positive and negative aerobic as well as anaerobic bacteria excluding the nonfermenters, MRSA and drug-resistant enterococci. E
Effective against most resistant enterobacteriaceae producing ESBLs and/or AmpC-type β-lactamases. limited in vitro activity against P. aeruginosa and Acinetobacter species, not suitable for the empiric treatment of serious infections acquired nosocomially.
Recommended for prophylaxis of surgical-site infection following elective colorectal surgery. Unlike imipenem, ertapenem does not require co-administration with cilastin.
Doripenem
Doripenem was approved for use by the FDA in 2007. Its spectrum is more similar to that of meropenem and imipenem than of ertapenem. Thus, it is effective against gram-positive and negative aerobes and anaerobes including Pseudomonas aeruginosa, Acinetobacter species, but not MRSA, VRE and other strains resistant to imipenem and meropenem. It is effective against β-lactamase producing strains of enterobacteriaceae
Doripenem is approved for the treatment of intra-abdominal infections and complicated urinary tract infections including pyelonephritis.
Dosage adjustment is required in renal failure patients.
Beta Lactamase Inhibitor
β-lactamase inhibitors In β-lactam agent/β-lactamase inhibitor combinations, the latter potentiates the action of the former by protecting it from enzymatic hydrolysis.
Currently used β-lactam/β-lactamase inhibitor compounds are highly active against class A and various ESBLs, but with poor activity against class C and class D enzymes.
Their main advantage over the older available β-lactamase inhibitors is conferred by the ability to inhibit class C and D enzymes. Thus, MIC of various currently used β-lactams, such as piperacillin or ceftazidime, is decreased when administered together with novel β-lactam inhibitors, these antibiotics become active against ESBL-producing strains.
Moreover, used combined with carbapenems, makes the latter active against MBL-producing strains.
Avibactam (also known as NXL104) is a β-lactamase inhibitor that has no antibacterial activity, but has interesting property to inhibit beta-lactamases. Currently it is in clinical development combined with both ceftazidime Bassetti et al.and ceftaroline. It displays a broad-spectrum inhibitory profile against enzymes belonging to classes A and C β-lactamases (including AmpCs, ESBLs, and KPC) [52], on the other side, in combination with aztreonam it offers a potential option against bacteria producing NDM-1 [53]. There are several on-going studies in phase III, assessing the efficacy in association with ceftazidime in the treatment of cIAI, HAP and cUTI [54,55]. mMK-7655 is a novel beta-lactamase inhibitor under clinical development. It displays good in vitro activity against class A and class C carbapenemases, especially when combined with imipenem/cilastatin. Currently the drug is in phase II clinical development trial for the treatment of cIAI and cUTI.
ME1071 (CP3242), a class-B inhibitor, maleic acid derivative,is a novel specific inhibitor for metallo-β-lactamases (MBL). It reduces the MICs of carbapenems for bacteria with NDM-1 enzyme. It can potentiate the activity of carbapenems (expecially biapenem) and ceftazidime against MBL-producing strains of P. aeruginosaand other Gram-negative bacteria, as E. coli, Serratia marcescens, A. Baumanii and K. pneumoniae. It shows less activity
Newer macrolides and ketolides
Newer macrolides and ketolides include:
In clinical use: Fidaxomicin, telithromycin
Ketolides are derivatives of macrolides with replacement of L-cladinose on the macrolide ring with a 3-keto group.
Newer macrolides and ketolides approved for use
Fidaxomicin
Fidaxomicin is probably the latest antibacterial approved for use in May 2011.
Indicated- Clostridium difficile-associated diarrhoea. Rates of recurrence for some strains of Clostridium difficile have also been found to be lower with fidaxomicin as compared to vancomycin in clinical studies.
Preferred drug in cases of recurrence.
MOA- Bactericidal- inhibiting bacterial RNA polymerase.
It is minimally or not absorbed following oral administration, thus systemic side effects are reduced.
It does not affect the normal flora of the lower gastrointestinal tract since it does not show any activity against gram-negative organisms.
Telithromycin – withdrawn for severe side effects
Newer tetracycline-related antibacterials
Newer antibacterials related to tetracyclines include:
In clinical use: Tigecycline In clinical trials: PTK-0796.
Tigecycline
Glycylcycline – structural derivative of minocycline. Approved for use in the year 2005 for complicated skin and soft-tissue infections, community-acquired bacterial pneumonia and complicated intra-abdominal infections. Its efficacy against gram-negative as well as positive organisms makes it a useful drug in mixed infections.
Tigecycline also shows potent activity against a number of resistant organisms.
MOA- binds avidly to the ribosome and does not undergo active efflux easily in gram-positive organisms. However, it is susceptible to efflux from organisms like Pseudomonas aeruginosa, Proteus spp., Providencia spp., and Morganella spp., which makes these organisms inherently drug resistant to tigecycline. MIC90 values for A. baumannii of 1-2 mg/L have been reported to be the lowest among all antimicrobials including carbapenems.
Dosage reduction may be required in severe hepatic impairment. It has excellent tissue penetration, thus supporting its use in deep tissue infections.
Gastrointestinal adverse effects like nausea, vomiting, diarrhoea and heartburn are commonly observed with tigecycline. It is contraindicated in pregnancy and children below 8 years of age.
Newer trimethoprim-related Drug
recently been accepted as New Drug Application by the FDA for the treatment of complicated skin and soft-tissue infections.
Iclaprim, a dihydrofolate reductase inhibitor, is being developed as a single agent, though it does show synergistic effect when administered with some sulfonamides.
Spectrum- S. aureus and S. pneumoniae, including several resistant strains. Its effectiveness against H. influenzae, Moraxella catarrhalis and Legionella pneumophila may also make it useful in respiratory tract infections. It is being developed as an intravenous as well as oral formulation.
Iclaprim has undergone Phase III trials