Urinary Tract Infection (UTI) : Etiopathogenesis and Lab Diagnosis
2 Anatomic Categories:
1. Upper UTI:
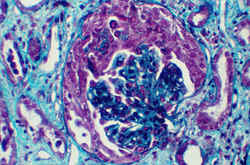
- Acute pyelitis (renal pelvis)
- Acute pyelonephritis (renal parenchyma)
2. Lower UTI:
- Cystitis (urinary bladder)
- Urethritis (urethra)
Predisposing Factors:
- Obstruction of urinary flow: Benign Prostate Hypertrophy, Calculus, Tumor, etc.
- Surgery: on the kidney or urinary tract
- Catheters: inserted through the urethra into the bladder
- Diabetes Mellitus and Immunocompromised states
- Vesicoureteral reflux (VUR): Reflux of urine from bladder up into ureters and renal pelvis
- Neurogenic bladder or Bladder diverticulum
- Female gender: Incidence in female is greater in male due to
- Proximity of urethra to anus: Colonization by colonic organisms
- Short length of urethra: About 4 cm
- Sexual intercourse: Introduction of bacteria into the bladder
- Use of diaphragm: Method of contraception
- Bladder or uterine prolapsed: Postmenopausal
- Pregnancy: Upper UTI is common in pregnancy due to
- Dilation of ureters and renal pelvis
- Stasis in right ureter
- Atony in ureteric musculature
- Incompetence of vesicourethral valves leading to VUR
- Congenital abnormalities in Infants
Common causative agents:
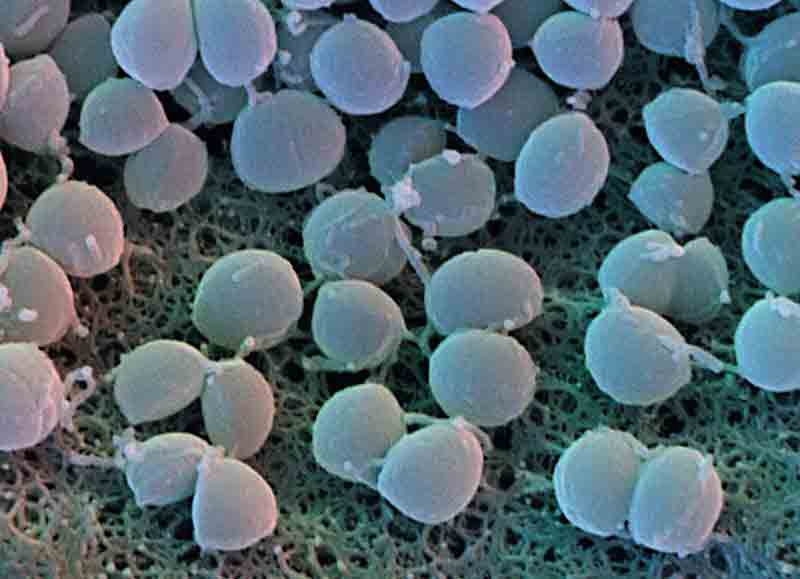
- Escherichia coli (Commonest etiology)
- Klebsiella
- Proteus mirabilis and other species
- Staphylococcus saprophyticus
- Enterococci (Group D Streptococci)
- Pseudomonas aeruginosa
Infrequent causative agents:
- Enterobacter, Citrobacter, Staphylococcus aureus
- Candida albicans
- Adenovirus type 2
- Increased ability to adhere to urethroepithelial cells: Fimbriae
- Increased resistance to serum cidal activity
- Hemolysin
- Urease
- Bacterial motility
- Endotoxin production
Mode of Infection:
- Ascending infection
- Hematogenous route
Clinical Manifestations:
- Urinary frequency
- Dysuria (painful burning sensation on urination)
- Hematuria (blood in urine)
- Suprapubic pain along with loin pain and tenderness
- Fevers and chills
LABORATORY DIAGNOSIS
A) Specimen Collection:
1. Midstream clean-catch technique/MSU (commonest method):
- Simple, inexpensive and noninvasive
- Cleansing of skin and mucous membrane adjacent to the urethral orifice before urination
- First part of urination is allowed to pass into the toilet
- Mid-portion of the stream is then collected in sterile container
- Disadvantage: Despite precautions, contamination of urine can occur
2. Straight catheter technique:
- Urine should be collected directly from the catheter and not from the collection bag
- Catheter should not be allowed to touch the container
- Disadvantage: Labor intensive, costly and invasive, risk of UTI
3. Suprapubic aspiration (rarely used):
- Best method to avoid contamination of specimen
- Disadvantage: Invasive, costly, time consuming, requires too much resources
B) Storage or Transport:
In case of delay in specimen processing (>2 hours), either of the following must be done:
- Storage: Refrigeration (4c) or Preservatives (Boric acid)
- Transport using Dip-slide method: Discussed below
C) Specimen processing:
1. Microscopic examination:
- Pyuria (Leukocytes in urinary sediment): >10/hpf is indicative of UTI
- Hematuria (RBCs and casts)
- Bacteriuria (Bacteria in uncentrifuged urine by gram stain): ≥1/hpf is indicative of UTI
2. Culture:
Routine culture media: Blood agar and MacConkey’s agar
Semi-quantitative culture:
- Standard loop technique: Calibrated loop is used to hold certain volume of urine which is cultured and incubated at 37c for 18-24 hours except in suspected funguria for which incubation is done for 48 hours to count colonies. Eg. If a loop can hold 0.004 ml of urine, then 250 loopfuls make 1ml. Hence colony count is expressed per 1ml by: 250 X Number of colonies in 1 loop
- Dip slides technique: Plastic slides coated with CLED (Cysteine lactose electrolyte deficient) agar on one side and MacConkey’s agar on the other side is dipped into freshly voided urine and replaced in a sterile container and incubated as in standard loop method. Viable count is obtaine by comparing growth on the media with the manufacturer’s chart.
Interpretation of results for different specimens:
1. MSU:
- ≥10^5 CFU/ml (Indicates UTI and sensitivity test is done)
- 10^3 to 10^5 CFU/ml (Indicates doubtful of UTI/contaminated and culture is repeated)
- ≤10^3 CFU/ml (Indicates contamination)
2. Suprapubic aspiration and Catheter: ≥10^2 CFU/ml (Indicates UTI)
D) Identification of organism:
a) Urine Biochemistry:
- Proteinuria
- Blood
- Nitrite (Nitrate reduction) test: In Enterobacteriacea associated UTI
- Leukocyte esterase test
b) Antimicrobial susceptibility testing:

3 Comments
Thanks for letting us know. It was useful. However, this can also spread through unhygienic public toilets. We must take care while using public toilets & use some highly effective & safe toilet seat sanitizer sprays available in the market. Or we can also make use of disposable toilet seat cover.
it was helpful !
thanx a lot ~
Nice to know that it helped you
Comments are closed.