Pathogenesis of Septic Shock
Shock (Cardiovascular collapse)
It is the final common pathway for a number of potentially lethal clinical events, including severe hemorrhage, extensive trauma or burns, large myocardial infarction, massive pulmonary embolism and microbial sepsis.
Regardless of the underlying pathology, shock gives rise to systemic hypoperfusion caused by reduction either in cardiac output or in the effective circulating blood volume.
Stages of shock
- Non-progressive phase (Early shock): Reflex compensatory phase (activation of renin-aldosterone-angiotensin system, increased ADH secretion, catecholamine secretion) is activated and perfusion of vital organs is maintained.
- Progressive phase (Late shock): Tissue hypoperfusion and onset of worsening circulatory and metabolic imbalances (Fall in blood pressure, diverted blood flow to brain & heart, fall in urine output and acidosis)
- Irreversible phase: Occurs after the body has incurred cellular and tissue injury so severe that even if the hemodynamic defects are corrected, survival is not possible (death due to multiple organ failure).
Morphology of Shock
- Brain: Ischaemic encephalopathy
- Heart: Coagulative necrosis or subendocardial haemorrhages
- Kidneys: acute tubular necrosis
- Lungs: “Shock lung” (diffuse alveolar damage -ARDS) occurs only in septic shock
- Adrenals: Cortical cell depletion
- GIT: Patchy mucosal haemorrhages and necroses (hemorrhagic enteropathy)
- Liver: Fatty change and central haemorrhagic necrosis (when severe)
Types of Shock
a) Cardiogenic shock
Clinical examples: Myocardial infarction (MI), Arrhythmia, Pulmonary embolism, etc.
Principal mechanisms: Failure of myocardial pump owing to intrinsic myocardial damage or extrinsic pressure or obstruction to flow
b) Hypovolemic shock
Clinical examples: Hemorrhage and fluid loss (vomiting, diarrhea, etc.)
Principal mechanisms: Inadequate blood or plasma volume
c) Septic shock
Septic shock results from spread and expansion of an initially localized infection (eg. abscess, peritonitis, pneumonia) into bloodstream.
Clinical examples:
- Overwhelming microbial infections
- Endotoxic shock (most cases) : caused due to endotoxin (LPS) producing gram negative bacteria
- Gram positive septicemia
- Fungal sepsis
- Superantigens (as in Toxic Shock Syndrome)
Principal mechanisms:
- Peripheral vasodilation and pooling of blood
- Endothelial activation/injury
- Leukocyte-induced damage
- Disseminated Intravascular Coagulation (DIC)
- Actication of cytokine cascades
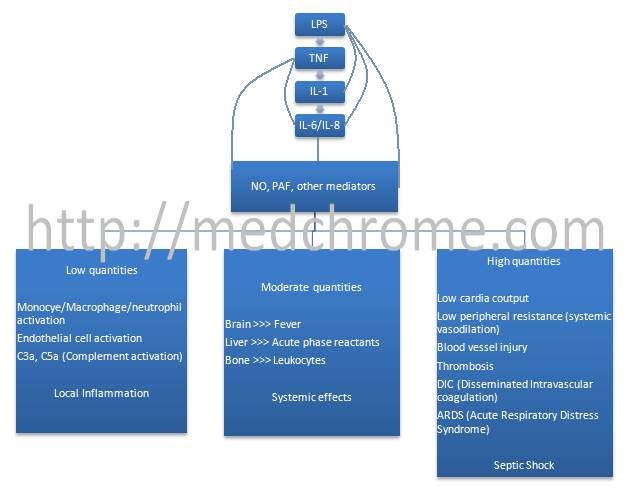
Pathogenesis of septic shock:
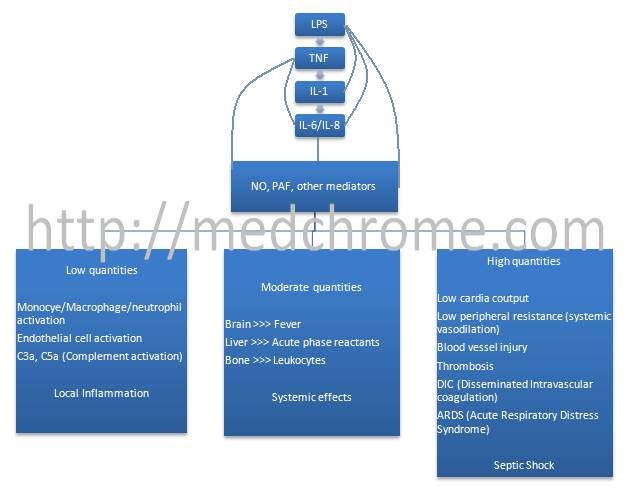
LPS –> circulating LPS-binding protein –> Complex –> binds to CD14 –> LPS binds to TLR-4 receptor
Engagement of TLR-4 on endothelial cells cause down regulation of natural anticoagulant mechanisms and when engaged on monocytes and macrophages, it causes profound mononuclear cell activation leading to production of IL-1 and TNF (Cytokines).