Mycobacterium tuberculosis
Mycobacterium Tuberculosis Complex (MTC):
- Mycobacterium tuberculosis
- Mycobacterium bovis
- Mycobacterium microti
- Mycobacterium africanum
- Mycobacterium canettii
General Characteristics:
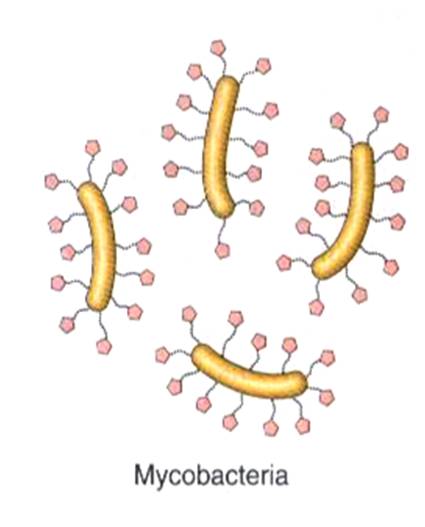
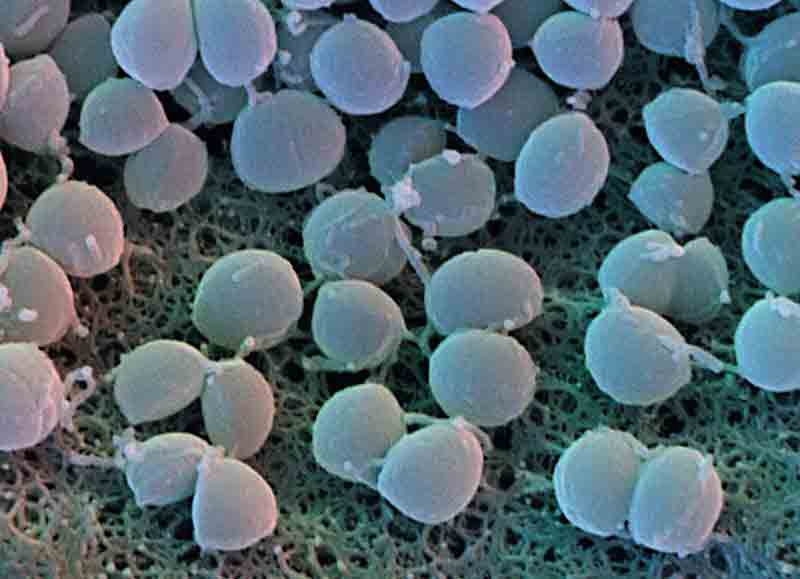
 Nonmotile, nonsporing and noncapsulated bacillus arranged singly or in group
Nonmotile, nonsporing and noncapsulated bacillus arranged singly or in group- Has a complex peptidoglycan arabinogalactan mycolate cell wall that is approximately 60% lipid, resulting in acid-fastness, poor Gram staining (weakly gram positive), and resistance to drying and many chemicals
- Mycobacterium tuberculosis appears slender, straight or slightly curved rod with beaded or barred appearance in ZN stain while Mycobacterium bovis appears straighter, stouter and shorter with uniform staining.
- A slow grower (generation time 12-24 hours) because it has single copies of ribosomal genes.
- Obligate aerobe and Facultative intracellular
Determinants of pathogenecity (Mycosides):
Mycosides are glycolipid derivatives of mycolic acid. Following mycosides are pathogenic determinants:
1. Cord factor (Trehalose mycolate):
- inhibits neutrophil migration and causes the organism to grow in a cord or serpentine fashion in culture
- elicits granuloma formation
- disrupts mitochondrial membranes, interfering with respiration and oxidative phosphorylation
- immunogenic
- release of TNF (cachectin) resulting in rapid weight loss in mice experiments
2. Sulfatides (Sulfur containing glycolipid):
- potentiates action of Cord factor
- permits intracellular survival in macrophages by inhibiting phagolysosome formation and by suppressing superoxide formation
3. Wax D (complex mycoside):
- activation of cell mediated immunity
Mnemonic: Mike WaxeD his SUrfboard and Corded (leashed) it
Mike: Mycoside
Waxed: Wax D
Surfboard: Sulfatide
Corded: Cord factor
Tuberculosis
Tuberculosis (TB) is an infectious bacterial disease caused by Mycobacterium tuberculosis, which most commonly affects the lungs. However, no organ is known to be spared by Tuberculosis, but it is extremely rare in pancreas, thyroid and muscles and unheard of in hair and nail.
Causative agent:
- Mycobacterium tuberculosis (hominis)
- Mycobacterium bovis
- Mycobacterium avium intracellulare (MAI)
Mode of transmission:
- Person to person transmission of airborne droplets of organisms from an active case to a susceptible host
- Oropharyngeal and intestinal TB due to drinking of M.bovis contaminated milk or swallowing sputum
- Transplacental route
Risk factors:
- Poverty, crowding and chronic debilitating illness
- Elderly
- Transplant recepient, AIDS, malignant disease, Diabetes Mellitus, Silicosis, Chronic renal failure, Malnutrition, Alcoholism, Immunosuppression due to corticosteroid
Pathogenesis:
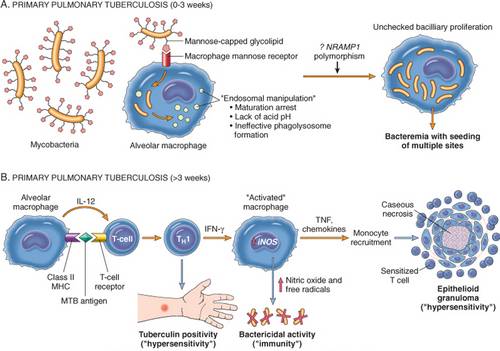
A. Primary Pulmonary tuberculosis:
Less than 3 weeks (Sensitization):
- Primary infection usually occurs in lungs of immunologically naive individuals. Inhaled bacteria land in the areas of the lung that receive the highest air flow: the middle and lower lung zones.
- Inhaled bacteria cause a local infiltration of neutrophils and macrophages
- The mycobacteria are picked up by phagocytic cells (macrophages) but the bacteria survives and replicates intracellularly due to endosomal manipulation mediated by virulence factors and kills the phagocytic cells.
- The bacteria spread through the lymphatics and bloodstream to to seed regional lymph nodes, other sites of lung and distant sites.
More than 3 weeks (Type 4 Delayed Hypersensitivity):
- Some macrophages succeed in phagocytosing the and breaking the invading bacteria.
- These macrophages then run toward a local lymph node and present bacterial antigens to T-helper cells.
- The sensitized T-cells leads to activation of macrophages which releases Nitric oxide and free radicals having bactericidal activity and mediators like TNF, chemokines which leads to granuloma formation.
- Caseous necrosis occurs in the center of the epitheloid granuloma. Viable organisms often remain on the outer edges of the necrosis, inside the granuloma.
Lesion: Ghon (Primary) complex comprising of Ghon focus (small focus of tuberculous pneumonia in lung parenchyma usually lower part of upper lobe or upper part of lower lobe) and nodal involvement (hilar lymphnodes and lymphangitis of draining lymph vessels). Ghon complex undergoes progressive fibrosis often followed by radiologically detectable calcification to form Ranke complex.
Clinical presentation: Mostly asymptomatic but symptomatic less frequently in children, the elderly, and the immunocompromised.
Fates:
- Healed lesions
- Latent lesions which can reactivate to progress to secondary TB
- Progressive primary TB leading to Milliary TB (small milliary tubercles containing numerous organisms but no caseous necrosis in different organs) due to massive lymphatic and hematogenous dissemination.
B. Secondary Pulmonary Tuberculosis:
- Secondary TB occurs either due to Reactivation of Latent lesion or Reinfection
- The infection can occur in any of the organ systems seeded during the primary infection. It is presumed that a temporary weakening of the immune system may precipitate reactivation.
- It normally reactivates in the upper lobe because oxygen tension is the highest there, due to decreased pulmonary circulation, and Mycobacterium tuberculosis is an aerobic bacterium.
- An old granuloma may weaken and erode into a bronchus or blood vessel (Progressive TB) and spread to take the form of Milliary TB.
Clinical presentation: Cough with hemoptysis (blood in sputum), night sweats, fever, anorexia and weight loss
Extrapulmonary Tuberculosis:
- Endobronchial, Endotracheal and Laryngeal TB
- Pleural and Pericardial effusion
- Tuberculous lymphadenitis or Scrofula (Commonest in cervical lymph nodes)
- Renal tuberculosis often presenting with sterile pyuria
- Pott’s disease of vertebra
- Tuberculous osteomyelitis
- Tuberculous meningitis
- Tuberculous salpingitis of fallopian tubes
Rule of 5 for Tuberculosis1. Droplet nuclei are 5 micrometers and contain 5 Mycobacterium tuberculosis bacilli.
2. Patients infected with Mycobacterium tuberculosis have a 5% risk of reactivation in the first 2 years and then a 5% lifetime risk.
3. Patients with HIV will have a 5+5% risk of reactivation per year.
Laboratory Diagnosis of TB
Specimen:
A. Pulmonary TB:
- Expectorated Sputum
- Induced Sputum
- Bronchoalveolar lavage
- Gastric lavage (Choice in children who cannot cough up the sputum)
- Lung biopsy
About collection of expectorated sputum:
- Early morning sputum with minimal saliva content of 3 consecutive days.
- Spot-Morning-Spot Timing is recommended now for non-hospitalized patients (i.e. Spot collection during initial visit to the clinic, Early morning sputum in the morning and Spot collection at second visit to the clinic) as it is more convenient.
B. Extrapulmonary TB:
- Urine: First-morning urine at least 50 mL, obtained by catheterization or from the midstream clean catch on
- three consecutive days for suspected Renal TB
- Fluids: spinal, pleural, pericardial, synovial, ascitic, blood, pus, and bone marrow
- Blood
- Tissue
Transport and Storage:
- Storage: 4 c for not more than 5 days
- Transport: Cetylpyridinium chloride (CPC) method
Detection
A. Microscopy:
1. ZN staining:
Reagents and Technique of ZN stain
Observation: Acid Fast Bacilli (AFB) appear as pink brightened rods
Significant bacterial count: 50,000 to 100,000 bacilli per ml of sputum
Quantitation scale recommended by WHO and International Union Against TB and Lung Disease
- 0: Report as Non AFB observed
- 1-9/100 fields: Report Exact count
- 10-99/100 fields: Report as 1+
- 1-10/field: Report as 2+
- >10/field: Report as 3+
2. Fluorescent staining:
- Stain: Auramine-rhodamine fluorescent stain
- Observation: Bright rods against dark background when examined under uv light
B. Concentration and Decontamination of Specimens:
Use: Smear, animal inoculation, culture
Techniques:
- Petroff’s method: sputum is liquefied with NaOH (4%), concentrated by centrifugation and then neutralized with HCl (8%)
- Homogenisation method: H2SO4, HCl or oxalic acid
- Trisodium phosphate method: Trisodium citrate, Sodium hydroxide, N-acetyl-L-cysteine (NALC)
C. Culture
Traditional Method:
1. Solid Medias: examined for growth twice a week for the first four weeks starting on day 3 to 5 postinoculation, and thereafter, once a week until the eighth week
Egg-based Lowenstein Jensen (LJ) media: Components of LJ media: To cook egg you need Egg (enhances growth), Salt (Mineral salt), Chilli (Malachite green inhibits contaminants), Sugar (Glycerol)
Agar-based Middlebrook 7H10 and 7H11 media
2. Incubation: 36-37 c in dark and light upto 12 weeks (Usually grow in 2 to 8 weeks)
3. Colony: Rough, tough and buff colored
4. Liquid medias: Liquid Media like Middlebrooke 7H9 media (Recovery of bacteria is quicker)
Newer method:
- Culture in Automated or Semi-automated liquid culture media like (Bactec 460)
- Radiolabeled broth demonstrating the metabolism of 14C-labeled palmitic acid with release of CO2
- Faster and more sensitive
D. Identification
Morphological properties: Microscopy and Colony characteristics
Biochemical tests
- Niacin test: Only M.tuberculosis produces niacin in sufficient quantities in egg medium to give positive test indicated by a canary yellow color.
- Catalase test: Tubercle bacilli (M.tuberculosis and M.bovis) are peroxidase positive and weakly catalsae positive while atypical mycobacteria are strongly catalase positive and peroxidase negative.
- Nitrate reduction test: Positive for M.tuberculosis but Negative for M.bovis
- Pyrazinamidase test: Positive for M.tuberculosis but Negative for other MTC species except M.cannetii
- Susceptibility to TCH (Thiopen-2-carboxylic acid hydrazide): M.tuberculosis is resistant but other MTC species except M.cannetti are susceptible
- Oxygen requirement: M.tuberculosis is aerobic but M.bovis is microaerophilic
E. PPD Skin Test:
- Reagent: Purified Protein Derivative (PPD) – purified preparation of antigenic tuberculoprotein
- Method: Mantoux test i.e. intradermal injection of 0.1 ml of PPD into flexor aspect of arm
- Purpose: A positive test indicates infection at some time but not necessarily current disease. This is important because many infected individuals will not manifest a clinical infection for years. When a positive PPD test occurs, you can treat and eradicate the disease before it significantly damages the lungs or other organs.
- Result: Read after 2-3 days
- Positive: Determined by measure of zone of induration
- 15 mm in a healthy person (not known to have exposure)
- 10 mm in individuals from countries of high risk, healthcare workers or after BCG vaccination
- 5 mm in HIV infected or with recent known exposure
- Flase negative:
- Milliary TB
- Aergic patients (Corticosteroids, malnutrition, Hodgkin’s disease, Sarcoidosis)
- False positive:
- BCG vaccination
- Atypical mycobacterium
F. Drug Sensitivity Testing: Using antitubercular drugs like Rifampicin, Isoniazid, Ethambutol, Pyrazinamide, Streptomycin, etc.



1 Comment
Really nice. Thank you Dr. Sulabh
Comments are closed.