Acute Peritoneal Dialysis
Indications in acute renal failure
Absolute:
1) Severe fluid overload with CCF
2) Severe hyperkalemia unresponsive to medical Rx or with ECG changes
3) Severe hyponeatrmia
4) Server metabloic acidosis requiring > 2 doses of NaHCO3 (2mEq/kg/dose)
5) Uraemia
6) Fluid restriction curtailling ample nutrition
Relative:
1) Anuria
2) High urea and creatinine values alone are not indications
METHOD
Materials:
1) Pertioneal dialysis tubing, trocar and cannula
2) Yellow intracath #14 gauge needle – 12 –24 inches long
3) Cut sown set with narrow blade
4) 2/0 silk on a straight needle
5) peritoneal dialysis fluid 1.5% dianeal (warm the fluid by placing in container of warm water
6) Lignocaine, Iodine, alcohol, mask and sterile gloves
Method: A
1) Consent form to be signed
2) Cross match 1 unit blood
3) Check PT, PTT platelets beforehand
4) Insert urethral catheter to empty bladder
5) Cleanse abdomen with Iodine and alcohol
6) Set up dialysis bags and attach to tubing (fluid should be tepid– not hot and not cold)
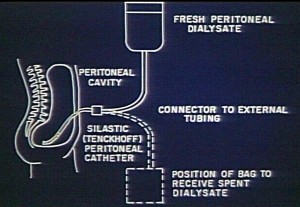
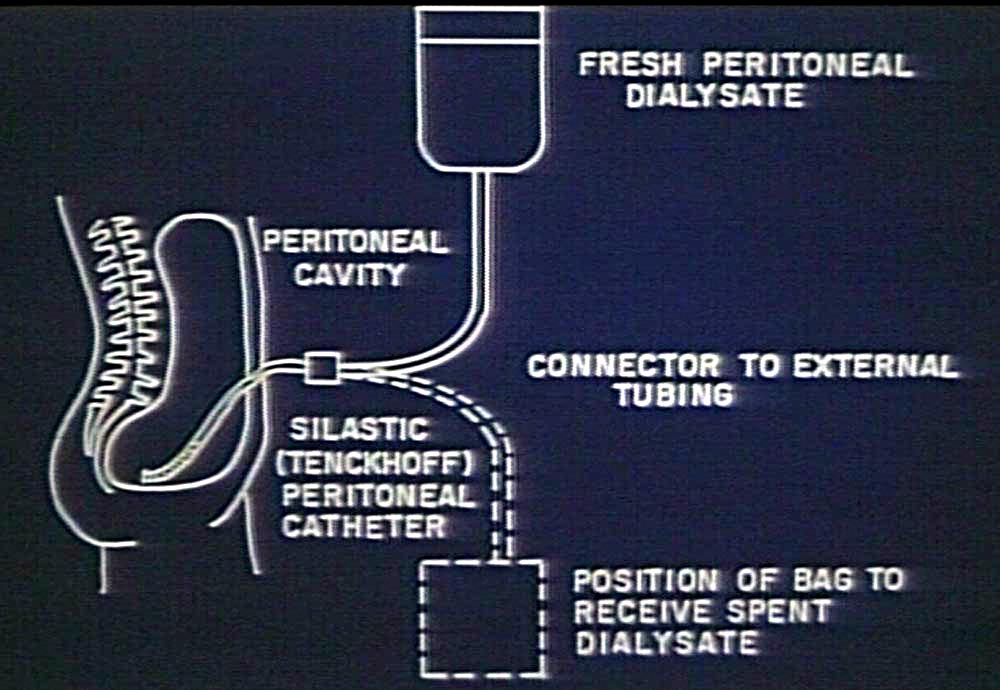
7) Determine, before dialysis starts, the volume to be run in and mark out on bag (See Figure 1).
The markings are not exactly in the same position on all bags, so this method is only an
approximation. If more accurate measurement is needed, a Biuretrol must be attached to the
dialysis bag
8 ) Fill tubing with fluid
9) If the abdomen is not tense with ascites, by infusing dialysis fluid until adequate tension is
present one reduces the risk of damaging internal structures eg aorta, inferior vena cava and
bowel. Proceed to step B
10) If the abdomen is already tense with ascites, proceed to step C
B
The procedure is as follows:
1) Remove guide wired from intracath
2) Set up tubing to dialysis fluid
3) Local anaesthetic to skin – superficial and deep at area of proposed intracath insertion
Direct the needle of the intracath downwards gently but firmly
When you feel the “pop” thread the tubing and withdraw the needle around it
Push tubing in as far as it will go – do not press deeply with the needle
4) Run in 30-50 cc/kg of dialysis fluid – sufficient to make abdomen tense
5) Withdraw intracath
6) Proceed to insertion of peritoneal dialysis catheter
C
Insertion of the peritoneal dialysis cannula:
1) Site of catheter – approximately 2 -3 cm inferior to the umbilicus and in the midline
2) Make a small incision at this point with the pointed end of the blade to include skin and subcutaneous
tissues – just big enough for catheter
Figure 1 – Dialysis bags and volume markings
85
3) Hold peritoneal dialysis catheter – with pointed trocar inside. Hand on top of catheter pushing
downwards firmly
4) When you feel the catheter enter the peritoneal cavity (a pop), remove the trocar (pointed internal
metal rod) and thread cannula (plastic part around the trocar) into peritoneal cavity quickly aiming the
cannula to the right or left iliac fossa (R preferably). Push in as far as it will go
5) Connect cannula (dialysis catheter ) to “elbow” and thus the remainder of tubing (already primed with
fluid)
6) Run out fluid from cavity into tubing – should run as a steady stream
7) Pour in expected exchange volume
a) 40-60cc/kg infants and small children
b) 30-40cc/kg older children
Limiting factors – abdominal discomfort, peritoneal leaks
8) If fluid runs in and out quickly after 3 rapid exchanges – without dwells – put purse string suture
around cannula – tie tightly, fasten securely at the level of the skin then tie 3-4 knots up the side of the
catheter with the same uncut suture
DIALYSIS
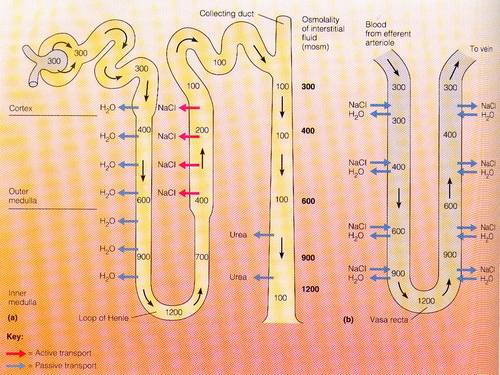
Cycles: Usually best clearance with 30 minute cycles :
• In over 5 minutes
• Dwell over 20 minutes
• Drain over 5 minutes
• Tepid fluid
Clearance: Urea > K > Cl > Na > Cr > PO4 > uric acid > HCO3 > Ca > Mg
Dianeal composition: Na 132 K 0 Ca 3.25 Mg 1.3 Cl 101.75 Lactate 35 mmol/l
Rate of water removal (assuming adequate drainage) depends on [glucose] in dialysis fluid
• 1.5% dianeal (1.5% glucose) usually adequate, but may increase to 2.5% or 4.25% if inadequat fluid
removal. If there is no pre-mixed 2.5 % or 4.25% dianeal, they can be prepared as follows
• to make 2.5% from 1.5% – add 40cc of D 50 W / 2 liters of fluid of 1.5% dianeal
• to make 4.25% from 1.5% – remove 110 cc fluid from 2 litre bag of 1.55 dianeal. Add 110 cc of
D50W to bag
ADDITIVES
1) KCl 6 mEq / 2 liters added when serum K <4.0mEq/l
– may be increased in increments of 2-4 mEq/2l bag depending on serum K
2) No antibiotics prophylatically
3) Heparin 1000 units /2 litres of dialysis fluid in all bags to minimize formation of fibrin strands
PERITONITIS
Initial broad spectrum cover for peritonitis.
Empiric therapies:
Intraperitoneal –
1) Cloxacillin 200mg/ 2litres + Gentamycin 10 mg /2 litres (regime used at UHWI with success despite
potential for inactivation when aminoglycosides mixed with penicillins) – Staph is commonest
pathogen for peritonitis here
2) Cefotaxime – 500mg/2 litres
Adjust when sensitivities available
Taken from “ Consensus guidelines for the treatment of peritonitis in pediatric patients receiving peritoneal dialysis” – Peritoneal Dialysis International Vol. 20: 610 – 624
PRECAUTIONS
• Daily peritoneal fluid: c/s, gram stain, cell count. > 100 WBC / ml and > 50% neutrophils suggests
peritonits. – start Rx as soon as sample taken for culture. Fluid is aspirated from the porthole (rubber
bung in tube in the dialysis line near patient entry) with a 25 gauge needle attached to a sterile syringe.
Clean the porthole with Iodine and wrap with Iodine soaked gauze for 10 minutes prior to inserting the
needle, in order to avoid iatrogenic peritonitis.*
• Nurse is asked to call if problems arise (see below)
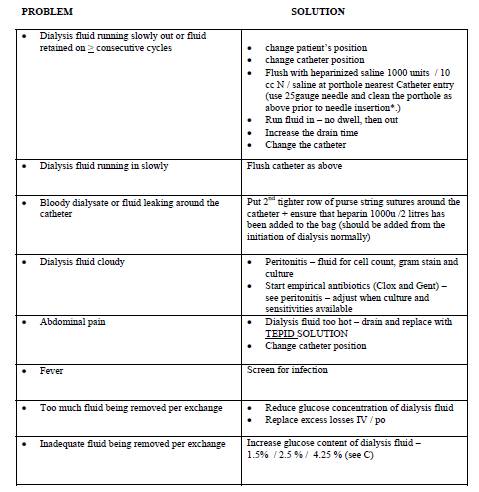
PROBLEM SOLUTION
Change PD catheter if unable to get good drainage or inflow despite the above measures. Always flush the
tubing with about 20 –50 cc of fluid as catheter is being withdrawn to minimize possibility of omentum
coming up in the catheter as it is being removed. Discontinue dialysis when urine output has improved
sufficiently that the original indications for dialysis are unlikely to recur off dialysis (not just when the lab
results are normal on dialysis
Source- Manual of Nephrology for DM
References:
1) ISPD guidelines / recommendations. Consensus guidelines for the treatment of peritonitis in pediatric
patients receiving peritoneal dialysis. Warady, Schaefer et al. Peritoneal Dialysis International 2000.
20:610 – 624.
2) Paediatric Nephrology (1997) 1: 183 – 194 (for drug dose adjustments)
3) Pediatric Nephrology 15th Edition (1999) Barratt and Vernier Chapter 69 (1125 – 1126)