Parkinson’s Disease: The Story of a Survivor

It was July 9th, 2005. Mr Joshi woke up at 4 am. He was feeling restless and did not know what to do. He had a bad dream. All the visuals and innuendos from the acrimonious discussions and meetings that had been happening in the office of late were rushing back to him that moment and creating a cacophony in his head. He had a glass of water and went to the washroom. He felt a bit tottery while returning to his bed but was too preoccupied to think about it. He tried hard going to sleep again but could not. Restless, he got up at 5 am and went for a stroll outside his residence. It was sultry in Delhi, but there was a cool bridge blowing as the monsoon had just started. He felt better.
Narendra Kumar Joshi, a trained Electrical Engineer and a Deputy General Manager with a Navratan Public Sector Company in India was 59 then. He was to retire from his job in a year’s time and felt the pressure of his job could actually force him to retire early. He used to feel glum and irritable at the office and his behavioural changes in office were spilling over into his family life as well. He started spending more time at lunch in the office as if to avoid going back to his cabin. He used to brood over the happenings around him. Even at dinner, his family members started pointing out to him that he was taking too much time finishing his meal. But as perseverant as he has been all his life, he carried on ignoring faint suggestions from his wife to consult a doctor.
It was January 27th, 2006 and Delhi seemed to be colder than ever before to Mr Joshi. He was gloomier than ever before that morning and did not feel like getting out of bed. The previous night, during a family gathering, he could not even speak properly with friends and relatives. He did not feel like speaking to them anymore, anyways. He overheard that somebody commented if he was drunk. He felt bad and had gone to his room early ignoring all requests to have dinner. He did not have an appetite, either.
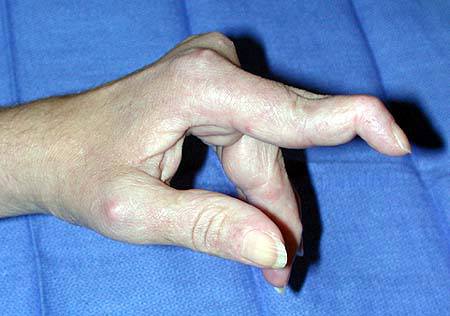
In the morning of Feb 1st, 2006, Mr Joshi summoned all his willpower and trudged to the washroom. It was already 7 am. He looked at the mirror and saw a glum, unshaven old man in it. He felt he should shave, which he had not done over the last 15 days or so. However, he could not hold the razor straight; the Delhi cold was getting onto him very weirdly that year he felt. He shaved but had a few cuts on both the cheeks and could not finish off properly. It was time to see the doctor know if something was wrong with him he felt.
The same day, at a private hospital in Delhi, Mr Joshi was diagnosed to be suffering from depression and stage 2 Parkinson’s disease.
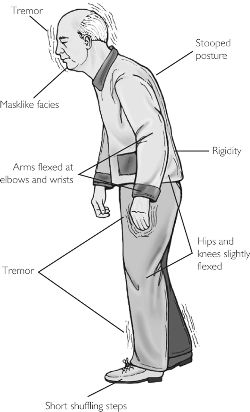
The symptoms of mood disorders and early stage Parkinson’s often overlap. In fact, anxiety and depression can be as prevalent in patients of Parkinson’s just as tremor and rigidity. Especially, depressive disturbances are common in patients with Parkinson’s disease and influence the clinical presentation of the disease. In addition to causing emotional distress, depression negatively impacts the quality of life, motor and cognitive deficits, and functional disability in patients with Parkinson’s disease. [Curr Neurol Neurosci Rep. 2013 Dec; 13(12): 409]. Persistent feeling of sadness, anxiety, hopelessness, irritability, guilt, worthlessness, or helplessness and a pervasive loss of interest or pleasure in hobbies and activities with decreased energy levels are common with depression, moving or talking slowly are also seen in many patients. In early stage Parkinson’s disease, tremor and other movement symptoms start occurring on one side of the body. Changes in posture, walking, loss of balance, slowness of movements and facial expressions start appearing slowly as the disease progresses.
Mr Joshi was put on Levodopa-Carbidopa combination and escitalopram. His symptoms improved; however, he continued to have sleep disturbances. Low dose clonazepam was added to his prescription two months later. Mr Joshi continued to improve on medication and retired from his job on 31st July 2006. Later he moved to Mumbai and from there to Brisbane, Australia in Oct 2006.
In Australia, the pollution free pleasant weather and the freedom from work pressure or liabilities did wonders to Mr Joshi’s health. He started following a rigid routine of morning walk for about 2 hours, followed by Yoga and Pranayam. He also started going on evening walks for another 2 hours every day. Although he was feeling way better than what he was at the start of 2006, during his stay in Australia he started enjoying life and health again. He started getting full control of his movements and could manage to shave, bathe and eat food in normal time. After a stay of 3 months when it was time to return from Australia, he decided to shift base to Indore, his native place.
In August 2007, after regaining full confidence in life and his health, Mr Joshi decided to take up a full-time consultant’s job in Mumbai. The job required him to travel to Dadar by local train, which he started doing without any problems whatsoever. All this while, apart from the travel, he was regular with the morning walks (40 minutes), Yoga (20 minutes) and Pranayam (20 minutes). He felt that sticking to a fixed health routine and the excitement of the new job improved his health further. In the meantime, while on a field trip to Jodhpur in 2009, he came across an Ayurvedic doctor who suggested him to take Chyavanprash, Ashwagandharisht and Dashmolarisht to boost his immunity. He started taking these ayurvedic products as well. Here’s an informative post about naturopathy vs ayurveda.
In 2011, five years after his diagnosis of Parkinson’s disease with depression his doctor in Mumbai changed his medication Ropinirole, a dopamine agonist and stopped all other modern medicines. By this time, he had started driving again and could do everything that a normal person of his age could do.
Currently, Mr Joshi is at the lowest dosage of Ropinirole and is devoid of any symptoms of Parkinson’s disease or of depression.
Analysis
Parkinson disease is one of the most common neurologic disorders, affecting approximately 1% of individuals older than 60 years. It causes a progressive disability that can be slowed, but, as per current research barring in a few exceptional cases, cannot be halted by treatment. The major findings in Parkinson disease are the loss of nerve cells in part of the brain called the substantia nigra leading to a reduction of a chemical called dopamine in the brain. Pathologists also find Lewy bodies within nerve cells.
Dopamine plays a vital role in regulating the movement and posture of the body. A reduction in dopamine is responsible for many of the symptoms of Parkinson’s disease. The cause for the loss of nerve cells is still unclear, though. The current concept is that genes and exposure to certain toxins or environmental factors combine together to cause the disease.
As the condition progresses, the symptoms of Parkinson’s disease generally get worse and it becomes increasingly difficult for the patient to carry out day-to-day activities without assistance.
As far as diagnostic tests go Parkinson disease is a clinical diagnosis. There are no laboratory biomarkers for the condition, and reports from routine magnetic resonance imaging (MRI) and computed tomography (CT) scan are invariably unremarkable for diagnosing the disease.
Fortunately, Mr Joshi was diagnosed at an early stage when intervention yielded immediate as well as a sustained result. Like, Mr Joshi, most of the patients respond well to treatment and only experience mild to moderate disability during a lifetime. A minority of patients, however, may not respond as well and progress fast towards severe disability. Although Parkinson’s disease doesn’t cause death directly, the condition can increase morbidity and can make patients vulnerable to life-threatening infections.
In conclusion, with advances in treatment, increased awareness about the condition and psychosocial support from family members and friends, most people with Parkinson’s disease can now have a normal or near-normal life expectancy. As Mr Joshi proved it, practising a healthy and active lifestyle can go a long way in warding off the disease.


Deputy General Manager & Senior Research Scientist
R & D, SRL Limited
Prime Square, Plot No.1, S. V. Road
Goregaon (West), Mumbai 400062, India