Health system in Nepal
According to WHO, a health system consists of all the organizations, institutions, resources and people whose primary purpose is to improve health. Health system in Nepal is 122 years old and based on Primary Health Care (PHC) approach.
HEALTH CARE SYSTEMS
A. Traditional Healthcare system:
- Without system: Dhami, Jhakri, Jharphuk, Gubaju, Tantrik, Lama
- With formal system: Ayurveda, Homeopathy, Naturopathy, Unani
B. Modern Healthcare system:
- Public sector
- Private sector: Profit and Non-profit
HEALTH SYSTEM ORGANIZATION
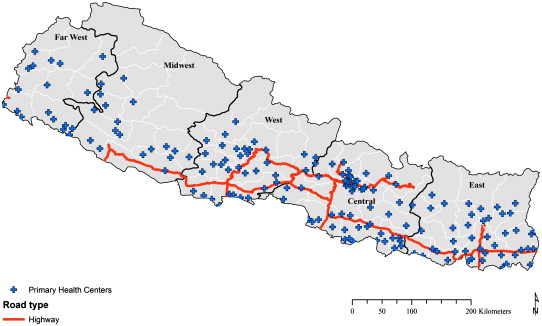
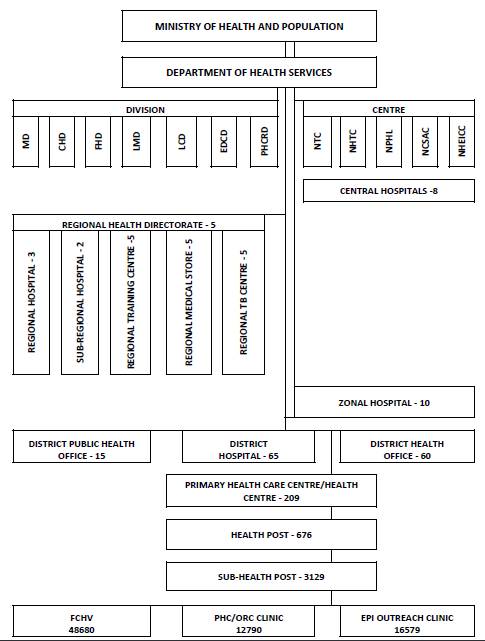
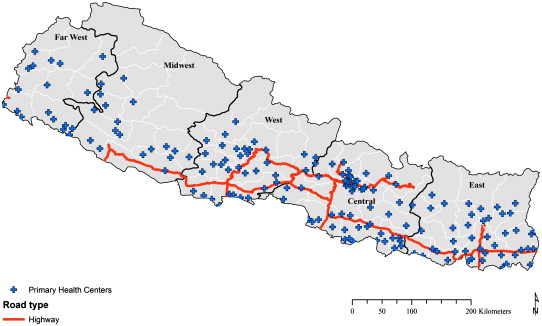
According to Annual report published by Department of Health Services (2010/2011) of Nepal, there are:
- 3,129 Sub-health posts (SHPs)
- 676 Health posts (HPs)
- 209 Primary Health Care centers (PHCCs)
- 65 District hospitals
- 10 Zonal hospitals
- 2 Sub-regional hospitals
- 3 Regional hospitals
- 8 Central hospitals
- 445 NGOs and 315 private health institutions
Levels of Healthcare
- Primary: SHPs, HPs, PHCCs
- Secondary: District hospitals, Zonal hospitals, Regional hospitals
- Tertiary: Central hospitals, Teaching hospitals
HEALTH GOVERNANCE
- Ministry of Health and Population (MoHP) consists of 3 departments: Department of Health Services (DoHS), Department of Ayurveda (D0A), Department of Drug Administration (DDA)
- 5 Regional Health Directorates (RHDs) directly under MoHP
- 61 districts are managed by District Health Office (DHO) with support District Public Health Office (DPHO), whereas the remaining 14 districts are managed by DPHO solely
- Facility level health/hospital management committees
- Regulatory bodies like Nepal Medical Council (NMC), Nursing council, etc.
National Public Health Laboratory (NPHL)
NPHL is a nodal institute for developing policy, guidelines and overall framework for capacity building in laboratory sector. Attention has been given in strengthening laboratory procedure and communication between national, regional and district levels and in strengthening the system ensuring the availability of essential equipment, logistics and human resources. At present there are 8 central hospital based laboratories, 3 regional hospital based laboratories, 2 sub regional hospital based laboratories, 11 zonal hospital based laboratories, 66 district hospital based laboratories, and 204 PHCC based laboratories in the country. In the private sector there are above 1,300 laboratories. NPHL is also conducting the laboratory surveillance activities on various disease pathogens such as Measles/Rubella surveillance, Japanese encephalitis surveillance, Influenza surveillance and Antimicrobial resistance surveillance.
Primary Health Care Revitalization Division (PHCRD)
PHCRD works towards reducing poverty by providing equal opportunity for all to receive quality and affordable health care services. This division is envisaged to revitalize PHC in Nepal by addressing emerging health challenges in close collaboration with other DoHS divisions and relevant actors. In 2067/68 monitoring committees were developed at all levels of health system; citizen charter were displayed in most of health facilities on EHCSs; trainings were conducted on rational drug prescription in 75 districts; integrated public health campaigns were organized in 8 districts and Peers Group discussion were conducted for rational use of drugs in 22 districts. PHCRD also provided transportation cost for marginalized community and senior citizen. Community Health Insurance piloting activities is continued in 8 PHCCs.
HEALTH MANPOWER
- Doctors
- Nurses/ANM (Auxillary Nurse Midwives)
- Paramedics/Health assistants
- Village Health Worker (VHW)
- MCHW (Maternal Child Health Workers)
- Ayurvedic Physician
- Vaidhya
- Female Community Health Volunteers (FCHVs) including Trained Traditional Birth Attendants (TBAs)
Note:
- Nepal currently has around 20 medical colleges (including both governmental and private)
- According to WHO, Regional average of physicians per 10,000 population is 5.6 and the same for Nurses and midwives is 10.9
- The major role of FCHV is to promote health and healthy behaviors of mothers and community people for the promotion of safe motherhood, child health, family planning, and other basic health services with the support of health personnel from the SHP, HPs and PHCCs. They also resupply OCPs, condoms, ORS packets, Vitamin A capsules and iron tablets and in IMCI programme disctricts, they also treat pneumonia and refer more complicated cases to health institution.
STAFFING PATTERN
A) PHC
- Medical Officer
- Health assistant
- Staff nurse
- Auxillary health worker (AHW)
- Auxillary Nurse Midwife (ANM)
- Lab assistant
- Cold chain assistant
- Village health worker (VHW)
- Kharidar/Assistant accountant
- Peon/Chaukidar
B) Health Post
- Health assistant/Senior AHW
- AHW
- ANM
- VHW
- Mukhiya
- Peon
C) Sub-health Post
- Sub-health post incharge
- VHW
- MCHW
- Peon
Role of Medical Officer (MO) in PHC
- Medical tasks: OPD checkup and management, Indoor management, Referral services, Drugs and supply management
- Organization and management: General administration, Personnel management, Planning, Staff meeting, Conflict management, Co-ordination with DDC, VDCs, political leaders and external stakeholders
- Financial management: Annual budget planning, Accounting and financial reporting
- Human resource development: Organize training, Represent the PHC in workshop and seminar within the district
- Supervision and monitoring of different programs
HEALTH FINANCING
- Private sector
- Government
- Foreing Donors and International NGOs
EVOLUTION OF HEALTH SYSTEM IN SOUTH ASIA
Traditional practices, often integrated with spiritual counselling and providing both preventive and curative care have existed for thousands of years and often coexist today with modern medicine. About 3 generations of health system reforms have occured in th 20th century.
1st generation (1940s and 1950s): People saw the founding of national healthcare systems and extension to middle income nations of social insurance systems.
2nd generation (from 1960s): The rising costs of hospital based care, its usage by better off, inaccessibility by the poor and rural population of even the most basic services led to promotion of PHC as a means of achieiving uthe affordable universal coverage. In 1978 PHC was adopted as the strategy for acheiving goal of “Health for all” by 2000. It had 8 elements, known as basic health care, to be conducted on the basis of equity, community involvement, appropriate technology and multi-sectorial approach. 8 original elements of PHC were:
- E: health Education
- L: Locally endemic disease control
- E: Expanded programme on immunization
- M: Maternal and child health care
- E: Essential drugs
- N: Nutrition
- T: Treatment of common disease and injuries
- S: Safe water and basic nutrition
3rd generation (current): “Health for All” was criticized for giving too little attention to people’s demand for health care. This led to a reform which is driven by the idea of responding more to demand, assuring access for the poor and emphasizing financing than just provision within the public sector. Health reform for the 21st century aims to achieve Health for All through People centered care.
MAJOR HEALTH PROGRAMME INITIATIVES
- Institutional delivery declared free with maternity incentive scheme
- Introduction of Free Health Care (service charges abolished and essential drugs provided for free)
- Surgery of uterine prolapse
- Cash support to poor patients suffering from cancer, heart disease, CKD, Alzheimer’s disease and Parkinson’s disease
- Compulsory 2 year posting of physicians (completing MBBS course in government scholarship) outside Kathmandu
- Community based neonatal care
- Nutrition supplemental porgramme
CHALLENGES
- Climate change and health
- Equity, accessibility, quality and coverage of essential health care services
- Nutrition
- Inter-agency co-ordination
- Sustainability of health programme
- Re-emerging and new emerging diseases
- Deployment and retention of Health manpower in remote and rural areas
- Increase in non-communicable diseases
Sources:



2 Comments
Sir plz post updated health care system and staffing pattern in secondary and tertiary level?
Sir Can you please update the recent health care delivery of Nepal as of 2075 BS?
Comments are closed.