Mechanical Ventilation Of Lungs
MECHANICAL VENTILATION OF LUNGS
Mechanical ventilation of lungs is carried out by intubating the patient by nasal or oral route or through tracheostomy and connecting endotracheal or tracheostomy tube to ventilator.

INDICATIONS:
- On the basis of blood gas analysis
- pO2<50mmHg in room air or pO2<60mmHg on FIO2 >.5
- pH< 7.25(acute respiratory failure)
- pCO2 >50mmHg
- pO2/FIO2< 250mmHg
- p(A-a)O2 gradient> 350mmHg on 100% oxygen
- On the basis of pulmonary function
- respiratory rate >35/min
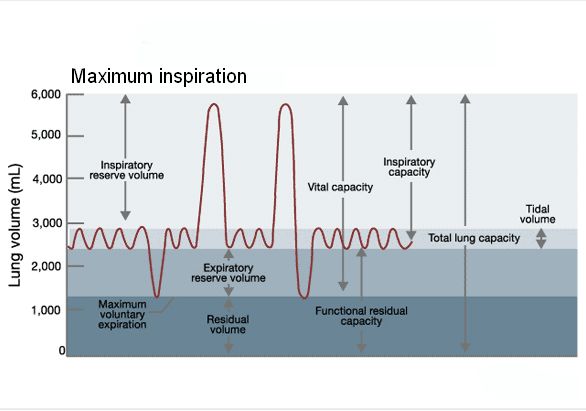
- vital capacity<15ml/kg
- dead space volume>0.6
- peak negative pressure -20cmH2O
- tidal volume <5ml/kg
- Other
- excessive fatigue of respiratory muscles
- loss of protective airway reflexes which makes patient vulnerable for aspiration
- inability to cough adequately
TYPES OF VENTILATORS
- TIMED CYCLED– these cycle to expiration once a predetermined time is elapsed since inspiration. Tidal volume is determined by set inspiratory flow and inspiratory time. These are used in operation theatres and in neonates.
- PRESSURE CYCLED– these cycle to expiration once predetermined pressure is reached. So if there is leak in circuit the predetermined pressure will not be reached and patient will remain in inspiration. Conversely if airway pressure is high there will be premature end of inspiration and patient can be hypoventilated so these ventilators are no more used
- VOLUME CYCLED– inspiration is terminated when a preset tidal volume is delievered. So theoretically the patient can not be hypoventilated even if lung compliance changes but actually this is not the case, a portion of tidal volume
(120-150ml) is lost in the ventilator breathing circuit and if patient’s pulmonary compliance is decreased the delievered tidal volume can further be decreased. So all these consideration should be kept in mind while setting the tidal volume and accurate tidal volume reaching the patient can only be calculated by putting spirometer at the endotracheal tube. These ventilators are most commonly used in ICUs.
SETTINGS OF VENTILATOR:
Typical ventilator settings are-
Tidal volume-10ml/kg ( current update: 5-8ml per kg)
Frequency- 10-12breaths/ min
I:E- 1:2
Inspiratory flow rate- 60-80 litres/min
Positive end expiratory pressure(PEEP)- 3-5 cm of H2O
Trigger sensitivity (for assist mode)–1 to -2 cm H2O
FIO2- 0.5

MODES OF VENTILATION:
- Controlled mode ventilation (CMV)/ intermittent positive pressure ventilation(IPPV) : in this mode patient’s own effort is nil. Only ventilator is delievering the preset tidal volume at preset frequency.
- Assist controlled ventilation: in assist control mode assist means the ventilator supplementation of patient initiated breath ( which itself does not have adequate tidal volume) and control means back up rate which is set up by clinician. So if patient’s spontaneous breath rate exceeds backup rate, no control breaths will be delievered and ventilator will purely behave in assist mode.
- Synchronized intermittent mandatory ventilation (SIMV): in this mode ventilator will deliever only between patient’s efforts or to coincide with the beginning of spontaneous effort i.e. synchronizing with the patient spontaneous respiration.
- Positive end expiratory pressure (PEEP): positive pressure is given at the end of expiration to prevent the alveoli to collapse and small airways to close, so that more time is available for gaseous exchange.
- Inverse ratio ventilation(IRV): ratio of inspiration to expiration is reversed(2:1). Prolonged inspiration will maintain positive pressure. So more or less it acts like PEEP. It is said to be better then PEEP and there is even distribution of ventilation.
- Pressure support ventilation: if a patient is on spontaneous respiration with adequate frequency but not adequate tidal volume, this mode is helpful in increasing the tidal volume.
- High frequency ventilation: this mode is applicable in conditions in which adequate tidal volume is maintained by high frequency
- Biphasic positive pressure ventilation(BIPAP): this is newer mode and is variation of pressure controlled ventilation and differs from conventional pressure controlled mode that spontaneous breathing is always possible
- Airway pressure release ventilation(APRV): applied to a patient on CPAP where there is periodic release of CPAP to decrease the incidence of barotrauma and hypotension.
COMPLICATIONS OF MECHANICAL VENTILATION
- 1. pulmonary barotraumas:
- incidence- 7 to 10%
- pneumothorax
- pneumomediastinum
- bronchopleural fistula
- pneumopericardium
- pneumoperitoneum
- air embolism
- 2. infection:
- pulmonary- due to prolonged intubation and frequent suction
- urinary- due to prolonged catheterization
- wound infection
- intravenous catheter related
- 3. complications due to prolonged intubation
- airway edema
- sore throat
- laryngeal ulcer and granuloma
- laryngeal web
- tracheal stenosis
- tracheal fibrosis
- 4. GIT:
- Stress ulcers
- Paralytic ileus
- 5. cardiovascular:
- right ventricular strain or even right ventricular failure
- 6. nosocomial infection
- liver and kidney dysfunction due to decreased cardiac output
- neuromuscular weakness– if muscle relaxants are used for longer periods
- ciliary activity– it is impaired if non humified oxygen is used.
10. oxygen toxicity– if higher concentration is used
11. psychological– depression and emotional trauma
12. due to prolonged bed rest–
- DVT and thromboembolism
- Bed sores
13. financial burden
WEANING FROM VENTILATOR:
It means discontinuing the ventilatory support.
Arbitrary guidelines for weaning are:
- pO2>60mmHg or O2 saturation >90% on FIO2<50% and PEEP<5 mmHg
- pCO2 <50mmHg
- respiratory rate <20/min
- vital capacity>15ml/kg
- Vd\Vt<0.6
- tidal volume > 5ml/kg
- minute ventilation<10litres/min
- inspiratory pressure<-30cmH2O
- arterial pH is normal
- normal haemoglobin
- norma cardiac status at the time of weaning eg at the time of weaning patient should not have tachycardia, hypertension
- normal electrolytes
- adequate nutritional status
METHOD OF WEANING:
From control mode ventilation patient is shifted to SIMV and then keep on decreasing the rate of breath delivered by ventilator gradually till it becomes 1 to 2 breaths/min. if the tidal volume is not sufficient then pressure supported ventilation may be instituted. The pressure support is decreased gradually till the patient achieves adequate tidal volume. Once the patient’s frequency and tidal volume is adequate then ventilator can be disconnected and T tube is attached to endotracheal tube. If patient is able to maintain normal pulmonary and cardiac function and shows normal blood gas analysis for more than 2 hrs, extubation can be attempted.

2 Comments
It is a nice attempt to summarise the vast topic on mechanical ventilation. It would definitely help the beginners and one has to understand that there remains a book hidden under each line read above. A few comments from my side are (also for beginners):
1) FiO2 at the beginning of MV should always be 100% and then should be gradually reduced to 60% over 6-8hours as the patient stablizes.
2) Thinking that SIMV is a weaning mode of MV is not correct. Patients can be gradually weaned even in assist control mode of MV (ACMV), which again is very different from the traditional control mode (CMV). CMV requires complete sedation and paralysis where as ACMV doesnt.
3) Patients can be kept in pressure support mode or T-piece which ever is tolerated better. No one method is superior than other.
4) If using SIMV mode, the minimum breaths delivered by the ventilator is usually 6, not 1-2.
5) Finally, if recent literatures are to be reviewed, there is ample evidence that SIMV mode is NOT a preferred mode of MV as it increases the work of breathing significantly and has no advantage over the ACMV mode.
Thanks,
Dr Binit Vaidya
MD (AIIMS), FACR
Lecturer,
NMCTH
Great post on this topic. Finally something I can read.
Comments are closed.