General Principles in Bacteriology Made Easy
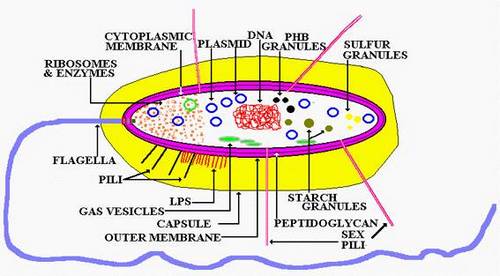
Bacterial Structures:
Size: 0.2 um (Mycoplasma species – smallest) to 5 um (Bacillus anthracis – largest) (compare RBC: 7um)
Peptidoglycan:
- Function: Gives rigid support, protects against osmotic pressure
- Chemical composition: Sugar backbone with cross-linked peptide side chains
Plasma (Cytoplasmic) membrane:
- Function: Site of oxidative and transport enzymes; semipermeable membrane
- Chemical composition: Lipoprotein bilayer beneath cell wall
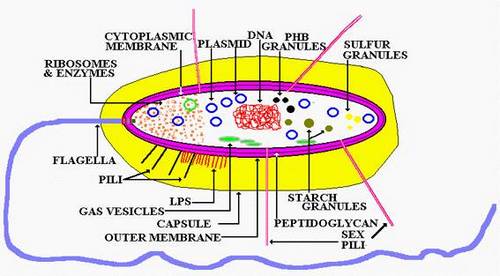
Cell wall (Gram positives):
- Function: Major surface antigen; freely permeable
- Chemical composition: Peptidoglycan for support and Teichoic acid induces TNF and IL-1
Note:
- 2 Layers:
- Inner cytoplasmic membrane
- Outer thick peptidoglycan layer (60-100% peptidoglycan)
- Low lipid content
- No endotoxin (except Listeria monocytogenes)
- No periplasmic space
- No porin channel
- Vulnerable to lysozyme and penicillin (penicillin binds to transpeptidase/penicillin binding protein)
Cell wall (Gram negatives):
- Function: Site of endotoxin (lipopolysaccharide); major surface antigen
- Chemical composition: Lipid A induces TNF and IL-1 and polysaccharide is the antigen
Note:
- 3 Layers:
- Inner cytoplasmic membrane
- Thin peptidoglycan layer (5- 10% peptidoglycan)
- Outer membrane with lipopolysaccharide (LPS)
- High Lipid content
- Endotoxin(LPS) present- lipid A
- Periplasmic space present
- Porin channel present
- Resistant to lysozyme and penicillin
Periplasmic space:
- Function: Space between the cytoplasmic membrane and outer membrane (cell wall) in gram negative bacteria
- Chemical composition: Contains many hydrolytic enzymes, including β-lactamases
Ribosome:
- Function: Protein synthesis
- Chemical composition: 70S ribosomes with 50S and 30S subunits
Capsule:
- Function: Surrounds bacterial cell wall and protects against phagocytosis by inhibiting complement (antiphagocytic virulence factor); antigenic (vaccine production)
- Chemical composition: Polysaccharide (except Bacillus anthracis, which contains D-glutamate)
- Encapsulated bacteria: Salmonella, Haemophilus influenzae type B, Influenzae type B, Neisseria meningitidis, Klebsiella pneumoniae, Streptococcus pneumoniae (Mnemonic: SHINKS)
- IgA protease producers: Streptococcus pneumoniae, Hemophilus, Influenza and Neisseria (SHIN)
- India ink stain: for Cryptococcus
- Quellung reaction: Can be detected by immunological method called Quellung reaction resulting in Capsular swelling
- Difference from slime layer: Slime layer remains detached from cell
Pilus/fimbria:
- Function: Adhesins; sex pilus formation during conjugation; hemagglutination
- Chemical composition: Glycoprotein
- Types: Common pili, Sex pili, Colicin Pili
- Gram negatives: Present only in some gram negative bacteria (Neisseria gonorrhea, E.coli, Campylobacter jejuni, Bordetella pertussis)
- Difference from flagella: Shorter and more numerous than flagella
Flagellum
- Function: Motility; Antigenic
- Chemical composition: Flagellin protein
- Parts: Filament, Hook and Basal body ( Basal body spans through the entire cell wall, binding inner and outer cell membrane in gram-negative and to inner membrane in gram positive bacteria)
- Flagellated organisms and Flagellar arrangement:
- Monotrichous (1 (polar) flagellum at 1 end): Vibrio cholera, Pseudomonas
- Lophotrichous (Multiple (polar) flagella at 1 end): Spirilla
- Amphitrichous (1 flagella each at 2 ends): Alkaligens fecalis
- Peritrichous (Multiple flagella over entire cell): Salmonella, E.coli, Proteus mirabilis
- Motility detection by direct microscopy in wet mount: Shows Brownian movement
Endospore:
- Function: Provides resistance to dehydration, heat, and chemicals (not reproductive because only 1 vegetative organism is formed)
- Chemical composition (From inside to outside): Cell membrane > Thick peptidoglycan mesh > Another Cell Membrane > Keratin-like protein > Exosporium
- Spore forming organims: 2 gram positive rods i.e. Bacillus and Clostridium
- Shape and position:
- Non-Bulging: Oval central, Spherical central, Oval subterminal
- Bulging: Oval subterminal, Oval terminal, Spherical terminal
- Sterilization destroys it while disinfection doesn’t
- Lab use: Sterilization control
Bacterial DNA (Nucleoid):
- Function: Replication; Antibiotic resistance genes
- Composition: Single circle of double stranded (ds) DNA without introns and RNA
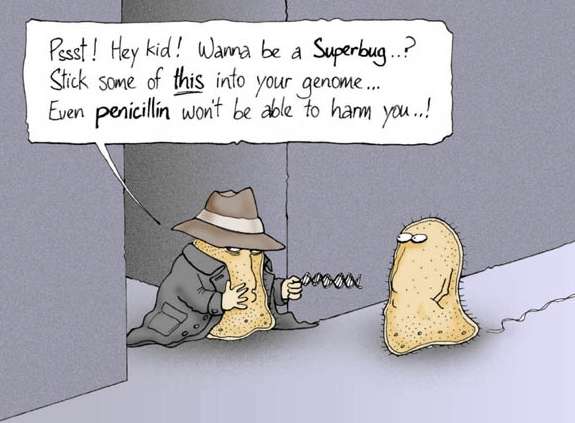
Plasmid:
- Function: Contains a variety of genes for antibiotic resistance, enzymes, and toxins.
- Chemical composition: ds, circular, supercoiled DNA (Plasmids are extrachromosomal DNA molecules)
- Properties: Self replication, may be self transferable, episomes can integrate with host chromosomes
- Types:
- Conjugative: Common in gram negative
- Non-conjugative: Common in gram positive
- Functional types:
- R-plasmids: RTF (Resistance Transfer Factor) and R determinant for Drug Resistance
- Col-factors: Bacteriocins (Colicin) from coliform bacterias
- F-factors (Fertility): Sex pili between F+ and F- cells for Conjugation
Glycocalyx
- Function: Mediates adherence to surfaces, especially foreign surfaces (e.g. indwelling catheters)
- Chemical composition: Glycoprotein
Structures of invasiveness
- In Shigella: Invasion plasmid antigens (Ipa) and Intracellular Spread protein (ICS)
Virulence factors:
- Protein A (S.aureus): bids Fc region of Ig and prevents opsonization and phagocytosis
- IgA protease (capsulated SHiN organisms):cleaves IgA to colonize respiratory mucosa
- M protein (group A streptococcus): prevents phagocytosis
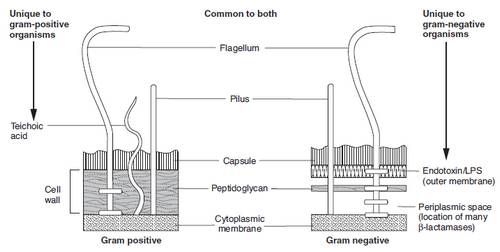
Bacterial Morphology:
Gram positive:
- Staphylococci
- Streptococci
Gram negative:
- Neisseria
2) Bacillus (Rod)
Gram positive:
- Clostridium
- Corynebacterium
- Bacillus
- Listeria
- Mycobacteria (Acid Fast)
Gram negative
- Enterics (Live in the GI tract):
- E. coli
- Shigella
- Salmonella
- Yersinia
- Klebsiella
- Proteus
- Enterobacter
- Serratia
- Vibrio
- Campylobacter
- Helicobacter
- Pseudomonas
- Bacteroides
- Haemophilus
- Legionella (silver)
- Bordetella
- Yersinia
- Francisella
- Brucella
- Pasteurella
- Bartonella
- Gardnerella (gram variable)
3) Braching filamentous (like fungi)
Only gram positive:
- Actinomyces (anaerobic)
- Nocardia (partly acid fast)
4) Pleomorphic
Only gram negative:
- Ricketssiae
- Chlamydia
5) Spiral
Only gram negative spirochetes:
- Treponema
- Borrelia
- Leptospira
6) No cell wall
- Mycoplasma
Gram’s stain:
Steps (CIDS):
- Crystal violet for 1 min in a heat fixed smear followed by washing off
- Iodine (violet color) for 1 min and then wash off
- Decolorise with alcohol or acetone for 10 to 30 sec and then wash off
- Safranin (pink color) as counterstain
Observation (microscopy):
Gram positive: appear violet due to retention of dye-iodine complex; hence safranin doesn’t enter the cell
Gram negative: appear pink because dye-iodine complex moves out and safranin moves inside the cell
Organisms:
All cocci except neisseria and branhamella are gram positive
All bacilli except Corynebacterium, Actinomyces, Nocardia, Bacillus, Mycobacterium, Listeria, Clostridium are gram negative (Mnemonic: Corny Actors Knock Back My Listerine in the Closet)
Limitations:
- Spirochetes (gram negative but too thin to be visualized) – hence demonstrated with darkfield microscopy and fluorescent antibody staining
- Rickettsia (intracellular parasite)
- Mycobacteria (high-lipid-content cell wall requires acid-fast stain)
- Mycoplasma (no cell wall)
- Legionella pneumophila (primarily intracellular)- demonstrated by silver stain.
- Chlamydia (intracellular parasite; lacks muramic acid in cell wall).
Mnemonic: Some Rascals May Microscopically Lack Color
Acid Fast Stain (Ziehl Neelsen or ZN stain):
Steps (CAM):
- Carbol fuschin (hot), a red stain for 10 minutes in fixed smear and then wash off
- Acid (Sulfuric acid 5% or 20%) as decoloriser for 1 min and then wash off
- Methylene blue 2% or Malachite green as counterstain for 2 min and then wash off
Observation (microscopy):
Acid Fast Bacilli (AFB) appear red in blue background of pus and epitheloid cells because they resist decolorization due to high content of Mycolic acid in the cell wall
Organisms:
Nocardia, Mycobacterium, Actinomyces, Cryptosporidium (Mnemonic: No, My Actor Cries)
Metabolic Classification
A) Oxygen utilization:
Bacteria posses 3 enzymes for this purpose:
- Catalase: breaks down hydrogen peroxide into water and oxygen
- Peroxidase: also breaks down hydrogen peroxide
- Superoxide dismutase: breaks down superoxide radical
1. Obligate aerobes: contains all 3 enzymes listed above
- Use and O2 dependent system to generate ATP (glycolysis, TCA cycle, ETC)
- Gram positive: Nocardia, Bacillus, Mycobacterium
- Gram negative: Neisseria, Pseudomonas, Bordetella, Legionella, Brucella
- Eg.: Nocardia, Pseudomonas aeruginosa, Mycobacterium tuberculosis, Bacillus Cereus (Mnemonic: Nagging Pests Must Breathe), Brucella, Legionella, Bordetella, Neisseria
2. Faculatative anaerobes: have catalase and superoxide dismutase
- They can grow in the absence of oxygen by using fermentation for energy. Thus, they have the faculty to be anaerobic but prefer aerobic conditions.
- Gram positive: Staphylococcus, Bacillus anthracis, Other grams positive rods excluding obligate aerobes
- Gram negative: Most gram negative rods excluding Obligate aerobes
- Mycoplasma
3. Microaerophiles (Aerotolerants): have superoxide dismutase but no catalase
- They can tolerate low amount of oxygen
- Eg.: Streptococcus, Spirochetes, Campylobacter
4. Obligate anaerobes: doesn’t have any of these enzymes
- Doesn’t use oxygen and cannot survive it
- Usually normal flora in GI tract and pathogenic elsewhere
- Eg.: Clostridium, Bacteriodes, Actinomyces (Mnemonic: Anaerobes Can’t Breathe Air)
B) Carbondioxide Utilization
- Capnophiles (CO2 loving): Neisseria (Meningococcus and Gonococcus), Brucellae
C) pH:
- Acidophil: Lactobacilli
- Alkalophil: Alkaligens fecalis
D) Obligate Intracellular Organisms:
- not capable of the metabolic pathways for ATP synthesis and thus must steal ATP from their host. These bacteria live in their host cell and cannot survive without the host like viruses.
- Eg.: Chlamydia, Rickettsiae
E) Facultative Intracellular Organisms:
- can live both intracellularly and extracellularly
- survive killing by leukocytes after phagocytosis through the inhibition of phagolysosome formation
- are safe from antibodies and other immune defenses inside cells where they replicate
- Eg. Salmonella, Neisseria, Brucella, Mycobacteria, Listeria, Legionella, Francisella (Mnemonic: Some Nasty Bug May Live Facultatively)
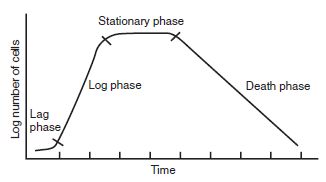
Bacterial Growth Cycle
Generation time: Population doubling time (An ordinary bacterium doubles 20-30 minutes by binary fission)
- Lag phase: Metabolic activity without division
- Log phase: Rapid cell division
- Stationary phase: Nutrient depletion slows growth and sporulation occurs in some bacteria
- Decline phase: Prolonged nutrient depletion and buildup of waste materials (toxins) cause death and involution forms may be seen
- Total count: Increases
- Viable count: Decreases
Products of Bacterial growth:
1) Toxins: Endotoxin and Exotoxin
A. Exotoxins:
Properties:
- Protein
- Heat labile
- Produced by
- Major gram positive bacterias except Listeria
- Gram negative bacterias like V.cholerae, E.coli, Sh.dysenteriae, V.parahemolyticus
- Strongly antigenic
- Highly toxic
- Filtrable
- Secreted by living cells
- Toxoid used as vaccines
- Encoded on plasmid or bacteriophage
Structure: In most exotoxins
- A (Active subunit): Cytotoxic
- B (Binding subunit): Binds A subunit to cell receptors
Types of Endotoxin:
1. Enterotoxins: Affects GIT to inhibit NaCl resorption, activate NaCl secretion, or kill intestinal epithelial cell causing infectious diarrhea or food poisoning.
Infectious diarrhea:
- Choleragen toxin: Vibrio cholerae
- E.coli Heat Labile Toxin (LT): E.coli, C.jejuni, B.cereus
- E.coli Heat Stable Toxin (ST): E.coli, Y.enterocolitica
- Shiga toxin: Shigella dysenteriae
- Shiga like toxin: Enterohemorrhagic E.coli, Enteroinvasive E.coli
- Toxin A: Clostridium difficile
Food posioning:
- Staphylococcal enterotoxin (types A-E)
- Bacillus cereus heat stable toxin
2. Neurotoxins: act on nerves or motor endplates to cause paralysis
- Tetanus toxin (Tetanospasmin): Clostridium tetani (Blocks the release of inhibitory neurotransmitters GABA and glycine)
- Botulinum toxin: Clostridium botulinum (Blocks the release of acetylcholine)
3. Pyrogenic toxins (superantigens): Bind directly to MHC II and T-cell receptor simultaneously, activating large numbers of T cells to stimulate release of IFN-γ and IL-2.
- Toxic Shock Syndrome Toxin-1 (TSST-1): Staphylococcus aureus (Toxic Shock Syndrome)
- Streptococcus pyrogenic/erythrogenic toxin (types A-C): Streptococcus pyogenes (Scarlet fever, Toxic Shock)
4. Cytotoxins: disrupts host cells in a variety of tissues
- Pseudomonas exotoxin A: Pseudomonas aeruginosa (affects liver)
- Diptheria toxin: C0rynebacterium diptheriae (affects heart, peripheral nerves and CNS)
- Tracheal cytotoxin: Bordetella pertusis (damages respiratory epithelial cells)
- Toxin B: Clostridium difficile (damages colonic epithelial cells)
5. Tissue invasive toxins: allow bacteria to destroy and enter through tissues
- Streptococcus pyogenes: Hemolysins/Streptolysins O and S, Streptokinase, DNAse, Hyaluronidase, NADase
- Staphylococcus aureus: Hemolysins, Staphylokinase, DNAse, Hyaluronidase, Lipase, Penicillinase, Leukocidin, Exfoliant (Stphylococcal scalded skin syndrome)
- Clostridium perfringens: More than 12 lethal toxins denoted by greek letters (alpha toxin- lecithinase, kappa toxin-collagenase, epsilon toxin-permease, etc.)
6. Miscellaneous Exotoxins:
Pertussis toxin: Bordetella pertussis (Causes exaggerated response to histamine and insuli and leukocytosis to cause Whooping cough)
Types by Mechanism:
1) Superantigens: S.aureus (TSST-1) and S.pyogenes (pyrogenic/erythrogenic toxin)
2) ADP ribosylating A-B toxins: B (binding) component binds to a receptor on A-B toxins surface of host cell, enabling endocytosis. A (active) component then attaches an ADP-ribosyl to a host cell protein (ADP ribosylation), altering protein function.
- Diptheria toxin: Inactivates elongation factor EF-2)
- Choleragen toxin: ADP ribosylation of G protein stimulates adenylyl cyclase and induces cAMP
- E.coli Heat Labile Toxin (LT): stimulates adenylate cyclase to induce cAMP
- E.coli Heat Stable Toxin (ST): stimulates guanylate cyclase
- Pertussis toxin: Induces cAMP by inhibiting Gαi
3) Others
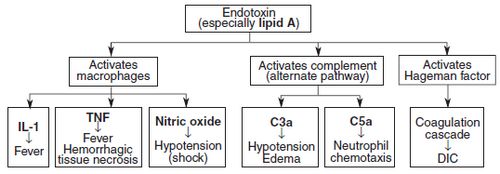
B. Endotoxins:
Properties:
- Lipopolysaccharide (LPS)
- Heat stable
- Produced by
- Most gram negative bacterias
- Listeria (Gram positive)
- Weekly antigenic
- Moderately toxic
- Not filtrable
- Structural part of bacteria released when lysed (release of large quantities due to lysis of bacteria following antibiotic use can cause septic shock)
- Cannot be converted to toxoids
- Encoded on bacterial chromosome
Structure: LPS is compsed of
- Outer O-antigen
- Central Core polysaccharide
- Innermost Lipid A: responsible for endotoxic activity
Mode of Action: IL-1 and TNF
- Fever (TNF mediated IL-1 release which leads to release of other cytokines and prostaglandins)
- Shock (TNF induced fall in blood pressure)
Some Diseases involving Endotoxins:
- Typhoid fever: Salmonella typhi
- Urinary Tract Infections: E.coli, Proteus, Klebsiella, etc.
- Meningococcal meningitis: Neisseria meningitidis
End-organ effects of Septic Shock:
- Cardiovascular: Vasodilation (Decreased blood pressure and organ hypoperfusion) and Decreased Cardiac output
- Kidneys: Acute renal failure (Decreased urine output, volume overload, accumulation of toxins)
- Lungs: Adult respiratory distress syndrome (Hypoxia)
- Liver: Hepatic failure (Accumulation of metabolic toxins, Hepatic encephalopathy)
- Brain: Encephalopathy (Altered mental status)
- Coagulation: Disseminated Intravascular Coagulopathy (Clotting and Bleeding)
2) Pigments:
- Actinomyces israelii: yellow sulfur granules (Israel has yellow sand)
- Staphylococcus aureus: golden yellow pigment (Aureus means gold)
- Pseudomonas aeruginosa: blue-green (pyocyanin) pigment (Aerugula means green)
- Serratia marcescens: red
Bacterial Pathogenesis
Terminologies:
- Pathogenicity: Ability of a class of bacteria to produce disease
- Virulence: Measure of degree of pathogenicity
- Infection: Lodgement and multiplication of infectious agent in the body
- Incubation period: Time interval between the entry of infective agent and the onset of clinical manifestations of disease
- Primary infection: First or initial infection caused by an infecting organism
- Reinfection: Subsequent infection by the same organism in the host
- Secondary infection: New infection in a host immunocompromised due to pre-existing infection by other organisms
- Cross-infection: New infection from patient or healthy carrier staff set up in an already diseased person
- Nosocomial infection: Cross-infection acquired in hospitals
- Iatrogenic infection: Physician induced infection resulting from drug therapy or diagnostic procedure
- Minimum lethal dose(MLD): Minimum number of bacterias/toxins required to kill a particular species of animal (inversely proportional to virulence)
- LD 50: Dose required to kill 50% of animals tested under standard condition
- Minimum infecting dose (MID): Minimum number of bacteria required to produce clinical evidence of infection in a susceptible animal (inversely proportional to virulence)
- ID 50: Dose required to infect 50% of animals tested under standard condition
- Attenuation: Reduction of virulence
- Bacteremia: Bacteria in the blood-stream. It is silent and transient without any bacterial multiplication and symptoms but can lead to septicemia when immune system is overwhelmed in host
- Septicemia: Clinical syndrome, which is accompanied by bacterial multiplication and the affected patient shows evidence of clinical sepsis (altered body temperature, elevation of WBC, increased heart rate or breathing rate)
- Pyaemia: Septicemia + formation of multiple abscesses
- Endotoxemia: Endotoxin circulates in blood
- Toxemia: Circulating blood contains only toxins, usually exotoxin
- Sapremia: Toxemia caused by certain toxin producing bacteria which are capable of growing in dead organic tissue (eg. Gas gangrene)
Steps in Bacterial pathogenesis:
1) Transmission: through various routes of infection from various sources
2) Adhesion: Adhesin-receptor interaction (Adherence of microbes to specific epithelial surface of host)
3) Invasion and Spread:
- Some bacteria reside on epithelial surface (noninvasive). eg. Vibrio cholera
- Some bacteria invade the cells but remains locally. eg. Shigella
- Some bacteria invade the cells and enter the bloodstream to reach systemic sites. eg. Salmonella typhi
4) Survival in the host:
Extracellular pathogens: evades phagocytosis through capsules (in most pathogens), protein A (S.aureus), M protein (S.pyogenes), etc.
Intracellular pathogens (obligate and facultative):
- live in cytoplasm by bypassing or lysing vesicles to avoid being killed by phagolysozomes or
- survive in phagosomes by inhibiting fusion of phagosomes with lysozomes (phagolysozome formation inhibition) or resisting degradative action of enzymes
5) Tissue injury:
- Exotoxins and Endotoxins
- Immunity
Culture of Bacteria
- Water/Broth = Liquid Media
- Agar/Medium = Solid Media
A) Simple (Basal) Media: used for routine culture
- Peptone water: Peptone + Water + NaCl
- Nutrient broth: Peptone water + Meat extract
- Nutrient agar: Nutrient broth + Agar
B) Complex Media:
1) General purpose medium:
- Glucose broth: Nutrient broth + Glucose (used for blood culture)
- Blood agar: Nutrient agar + sheep/horse blood (used for general culture)
- Alpha hemolysis (Incomplete hemolysis forming green ring around colonies): Streptococcus pneumoniae (optochin sensitive) and Streptococcus viridans (optochin resistant)
- Beta hemolysis (Complete and clear hemolysis): Staphylococcus aureus (catalase positive), Streptococcus pyogenes- group A streptococci (catalase negative and bacitracin sensitive), Group B streptococci (catalse negative and bacitracin resistant), Listeria monocytogens (tumbling motility)
2) Special Media:
- Tetrathionate broth: Enrichment culture for salmonella
- Selenite F broth: Enrichment culture for salmonella and shigella
- Desoxycholate citrate agar (DCA): Selective medium for Salmonella and Shigella
- Xylose Lysine Desoxycholate agar (XLD): Salmonella and Shigella
- Alkaline peptone water: Enrichement culture for vibrio
- Wilson and Blair Smith Sulphite Medium: Selective Medium for Salmonellae
- Chocolate agar (heated blood agar) with factors V (NAD) and X (hematin): Hemophilus influenzae
- Thayer Martin (VPN) Media: Neisseria gonorrhea
- Vancomycin inhibits gram positive organisms, Polymyxin inhibits gram negative organisms and Nystatin inhibits fungi; Hemoglobin enhances growth)
- Bordet-Gengou (Potato) agar: Bordetella pertussis (now replaced by Charcoal Blood Agar)
- Loeffler’s medium and Tellurite plate: Corynebacterium diptheriae
- Lowenstein-Jensen (LJ) agar: Mycobacterium Tuberculosis
- Components of LJ media: To cook egg you need Egg (enhances growth), Salt (Mineral salt), Chilli (Malachite green inhibits contaminants), Sugar (Glycerol)
- Dorset’s egg: Mycobacterium
- Eaton’s agar: Mycoplasma pneumoniae
- Mac-Conkey’s agar: Selective medium for Lactose fermenting enterics ( produce pink colonies)
- Components of MacConkey agar: Bile salts and crystal violet inhibit gram negatives and neutral red serves as indicator of lactose fermentation)
- Charcoal yeast extract agar buffered with cysteine: Legionella
3) Transport Media:
- Stuart’s media: Neisseria gonorrhea (gonococci)
- Bile peptone transport: Vibrio cholera
4) Anaerobic culture media:
- Thioglycollate broth
- Robertson’s cooked meat broth
Anaerobiosis (Anaerobic Culture Methods)
1) Displacement of oxygen:
- Candle (Displacement by inert gas)
- Vacuum dessicator
2) Absorption of oxygen:
- Pyrogallic acid
- Chromium (Cr) + H2SO4
- Gas-pak:
- Sodium borohydride + Cobalt chloride and Sodium bicarbonate + Citric acid with Almunium/Pallidum catalyst
- Generates H2 and CO2 when H20 is added and H2 produced combines with oxygen
3) Displacement and combustion of oxygen:
- McIntosh and Filde’s jar
- Catalyst: Pallidum or Platinum
- Principle: Slow combination of H2 and O2
- Indicator: Reduced methylene blue (colorless anaerobically but regains blue color on exposure to oxygen)
4) Biological methods:
- Using anaerobic organisms
5) Reducing agents in media:
- Thioglycollate broth: contains 0.1% thioglycollate
- Robertson’s cooked meat broth: contains cooked meat pieces
Microscopic Examination of Bacteria
1) Unstained Wet Mount or Hanging Drop preparation in Normal Saline:
- To study motility and distinguish motile from non-motile bacterias
- Positive result: Darting (vibrio cholera), zigzag, tumbling (Listeria) or other organized motility
- Negative result: No motility or Brownian movement only
2) Direct microscopy with Stained Smears:
- Gram stain: Gram positive and negative organisms
- Ziehl-Neelsen stain: Acid Fast Bacilli
- Giemsa stain: Borrelia, Chlamydia
- Silver stain: Legionella
3) Fluorescent microscopy with Stained Smears:
- Dyes (Fluorochromes): Auramine rhodamine, Acridine orange
- Observation: Stained bacteria become visible as a bright object against dark background
4) Dark Field Microscopy:
- For Spirochetes
Biochemical Tests for Bacteria
1) Break down of sugars
- Substrate: Glucose, sucrose, mannitol (For aerobic) and Lactose (For anaerobic – E.coli, Klebsiella, Enterobacter, citrobacter give positive result)
- Observation: acid (indicated by pink color) and/or gas
2) Voges-Proskauer (VP) test:
- Substrate: Glucose
- Observation: Deep pink color due to fermentation of glucose to neutral
3) Methyl red (MR) test:
- Substrate: Glucose
- Observation: Bright red reactions due to fermentation of glucose to acid (pH < 4.5)and negative reactions by yellow
4) Citrate utilization:
- Substrate: Sodium citrate
- Observation: Blue color in positive reaction and Green color in negative reaction
5) Indole test:
- Substrate: Tryptophan
- Observation: Red colored ring near surface
IMViC (Indole, MR, VP and Citrate utilization) test is used to differentiate the enterics.
Results:
- ++– : E.coli, Edwardsiella, Proteus vulgaris
- –++ : Klebsiella pneumonia, Enterobacter, Serratia
- -+-+ : Salmonella, Citrobacter freundii
- -+– : Shigella
- ++-+ : Citrobacter koseri
6) Hydrogen sulphide production:
- Substrate: TSI (triple sugar iron) agar
- Observation: Black color due to H2S production
- Positive in: Salmonella, Proteus, Edwardsiella, Citrobacter (SPEC)
7) Urease test:
- Substrate: Urea
- Observation: Pink color of medium due to production of ammonia
- Urease positive organisms: Proteus, Klebsiella, H.pylori, Ureaplasma (Particular Kinds Have Urease)
8) Oxidase test:
- Substrate: Redox dye
- Observation: Oxidation to purple color
- Positive in: Vibrio, Pseudomonas, Campylobacter, H.pylori, Exclude Enterobacteriacea (-ve test), Neisseria (Vice President CHEN)
9) Catalase test:
- Substrate: Hydrogen peroxide
- Observation: Oxygen (gas bubbles)
- Positive organisms: Staphylococcus, Pseudomonas, Aspergillus, Candida, Enterobacteriaceae (Catalse gives Breathing SPACE) and Neisseria.
10) Nitrate reduction:
- Substrate: Potassium nitrate
- Observation: Red color due to nitrite production
- Positive in: Serratia, E.coli, Enterobacter, Staphylococcus aures (SEES Nitrate)
Drug Sensitivity Tests
A) Disc diffusion method:
- Preparation of Medicated discs: Filter paper discs (6mm) with optimum amount of drug is dried and stored
- Preparation of Culture plate: Liquid culture of bacteria or urine is flooded on solid culture medium on a plate and excess is thrown away
- Medicated discs are placed on prepared cultured plate and incubated over night (18 hrs)
- Observation: Zone of inhibition in case of antibiotic sensitivity
- Examples: Stoke’s method, Kirby Bauer disc diffusion method
B) Tube dilution method:
- Serial tube dilutions of drug in broth are inoculated with bacterium under test and incubated
- Useful in determination of Minimum Inhibitory Concntration (MIC) and Minimum Bactericidal Concentration (MBC)
Bacterial Genetics
Mechanisms of Gene Transfer:
A) Transformation:
- Ability to take DNA from environment (also known as competence)
- Griffith experiment with Streptococcus pneumoniae
B) Conjugation:
- F+ cell= having Fertility factor and F- cell= not having fertility factor
- F+ X F- (F Plasmid replicated and transferred from F+ cell to F- cell)
- Hfr= F factor + Bacterial chromosome
- Hfr X F- (Transfer of F plasmid and chromosomal genes)
- F’ factor= Hfr – bacterial chromosome
- F’ X F- (Transfer of F plasmid with some DNA taken from bacterial chromosome)
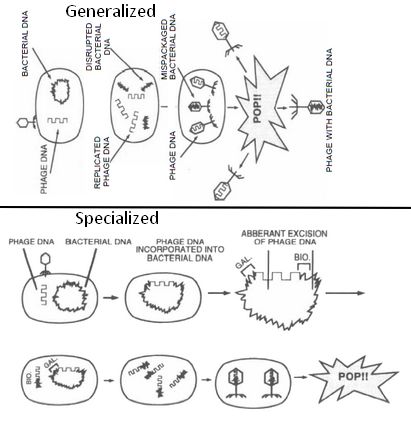
C) Transduction:
1) Generalized:
- A “packaging” event.
- Lytic phage infects bacterium, leading to cleavage of bacterial DNA and synthesis of viral proteins.
- Parts of bacterial chromosomal DNA may become packaged in viral capsid.
- Phage infects another bacterium, transferring these genes.
- Hence, in generalized transduction, there is transfer of any bacterial genes and phage DNA is not carried. It is involved in antibiotic resistance.
2) Specialized (Restricted):
- An “excision” event.
- Lysogenic phage infects bacterium; viral DNA incorporated into bacterial chromosome.
- When phage DNA is excised, flanking bacterial genes may be excised with it.
- DNA is packaged into phage viral capsid and can infect another bacterium.
- Hence, in specialized transduction, only genes immediately adjacent to site of prophage attachment is transfered. It is involved in transmission of virulence genes.
D) Transposition:
- Segment of DNA that can “jump” (excision and reincorporation) from one location to another, can transfer genes from plasmid to chromosome and vice versa.
- When excision occurs, may include some flanking chromosomal DNA, which can be incorporated into a plasmid and transferred to another bacterium.
Lysogeny: Genes for the following 5 bacterial toxins encoded in a lysogenic phage:
Mnemonic: ABCDE
- ShigA-like toxin
- Botulinum toxin (certain strains)
- Cholera toxin
- Diphtheria toxin
- Erythrogenic toxin of Streptococcus pyogenes
Types of mutation:
A. Point mutation:
a) Base pair substitution:
- Transition: One purine to other or One pyrimidine to other
- Tranversion: Pyrmimidine to purine or vice versa
b) Silent mutation:
- Codon I (encodes an amino acid – AA) –> Codon II (encodes same AA)
B. Frame shift mutation:
a) Missense mutation:
- Codon I (encodes an AA) –> Codon II (encodes different AA)
b) Nonsense mutation:
- Codon I (encodes and AA) –> UAA, UGA, UAG (nonsense codon terminates translation)
C. Multisite mutation: Deletion, Addition, Duplication, Inversion
D. Helix distortion
E. Suppression mutation
General Framework of Laboratory Diagnosis
1) Specimen collection
2) Transport in transport media or Storage at 4c if required during delay
3) Culture and Isolation
4) Identification:
- Microscopical morphology
- Cultural characteristics (Color, consistency, shape, size, surface, elevation, edge, opacity)
- Biochemical tests
- Agglutination tests
5) Animal inoculation test
6) Serology: Agglutination test, Complement fixation test, Flocculation tests, Indirect immunofluorescence
7) Molecular detection: DNA probes and PCR
Sources:
- A Textbook of Microbiology by P.Chakraborty
- Clinical Microbiology Made Ridiculously Simple (Medmaster)
- First for the USMLE Step I
- Various internet sources and poweroints


1 Comment
thanx alot…
Comments are closed.