AN APPROACH TO A CHILD WITH WHEEZE

WHEEZES OR RONCHI:
Wheeze is a dry musical sound associated with airway narrowing.
The expiration is prolonged.
WHEEZING:
Common in infants and young children because of unique age specific anatomic and physiologic properties and gender specific intrinsic lung characteristics.
- By year 1- 20% children
- By 3 years- 33% children.
- By 6 year- 50% children.
<15% children are subsequenctly diagnosed with Asthma based on symptom of recurrent wheezing airway.
TYPES OF WHEEZE:
- Monophonic Wheeze: Produced when there is localised obstruction of a bronchus. i.e Foreign body inhalation, hilar lymphadenopathy
- Polyphonic wheeze: Produced when there is generalized airway obstruction i.e Bronchial Asthma,Bronchitis.
CLASSIFICATION ON THE BASIS OF THEIR PITCH AND SITE OF ORIGIN
1) High pitch ronchi or Sibilant rhonchi:
Produced in the broncioles.
Audible during the end of inspiration or beginning of expiration.
Better apperciated by placing the chest piece in front of infant’s mouth and nose( acute bronchiolitis)
2) Medium pitch ronchi:
Produced in the medium sized bronchi.
3) Low pitched or sonorous rhonchi:
Produced in large bronchi.
Heard throughout both the phases of breathing.
Often audible without a stethoscope.
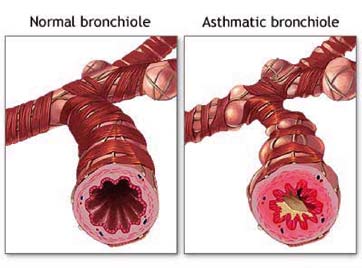
Pathophysiologic properties predisposing infant and children to wheeze
Decreased Broncial smooth muscle content – Decreased structural support
Hyperplasia of bronchial mucus – increased mucus production and risk of obstruction
decreased radius of conducting airways – decreased conductance
ed resistance in peripheral airways due to decreased airway size – increased risk of obstruction
Increased work of breathing.
CAUSES:
INFECTION:
- RSV
- Adeno virus
- influenza
- para influenza virus
- rhino virus.
- Others: tuberculosis,
- Chlamydia trochomatis
- Histoplasmosis.
ANATOMICAL ABNORMALITIES:
- laryngomalacia
- tracheomalacia
- vascular ring.
- medistinal Lymphadenopathy
- Tracheoesophageal fistula
- Laryngeal cleft.
- Broncheal /lung cyst
- Congenital heart disease with left to right shunt( increased pulmonary oedema)
ASTHMA:
Transient wheezer: onset ? 3 years then resolve.
- Initial risk factor is primarily diminished lung size.
- Normal lung function by 6 years of age.
- Not associated with increased risk of developing clinical asthma.
Persistent wheezer: onset? 3 years then persists.
Initial risk factor includes passive smoke exposure, maternal asthma history, elevated IgE level in 1st year of life.
Irreversible reduction in lung function at 6 yrs of age.
At increased risk of developing clinical asthma.
Late onset wheezer: onset between 3 to 6 years of age.
INHERITED:
cystic fibrosis.
Immune deficiency states
B cell deficiency
IgA deficiency
primary ciliary dyskinesia
Bronchiectasis
Neonatal AIDS
BRONCHOPULMONARY DYSPLASIA
ASPIRATION SYNDROME:
Gastro oesophageal reflux disease
Pharyngeal/s wallow dysfunction
INTERSTITIAL LUNG DISEASE INCLUDING BRONCHIOLITIS OBLITERANCE.
FOREIGN BODY ASPIRATION.
DIAGNOSIS
HISTORY:
Number and frequency of wheezing episodes.
Relationship of the episode to viral infection/aeroallergen exposure.
The presence of allergic disease such as conjunctivitis, rhinitis and or eczema, the parental history of asthma.
History of cough , chocking (foreign body intake.)
ON EXAMINATION:
Sign of respiratory distress and work of breathing.
Wheezing, transmitted upper airway nasal congestion,
Stridor and wheezing( suggestive of both upper and lower airway process such as croup tracheomalacia or bronchomalacia.
Crackles and wheezing(suggestive of interstitial lung component including infection and bronchopulmonary dysplasia or Pulmonary oedema with Congenital heart disease.)
ADDITONAL FINDINGS:
Childs growth curve: evidence of poor weight gain suggest of cystic fibrosis, immunodeficiency, GERD.
Clinical feature such as rhinitis,conjunctivitis,and presence of eczema(finding suggestive of atopy and risk factor for development of persistent wheezing.)
Presence of midline structural or cutaneous lesion such as haemangioma( associated with increased risk of intrathoracic lesion)
INVESTIGATION:
IMAGING: –
CHEST X- RAY: commonly used for diagnosis of pulmonary infection
CT SCAN: LNs, tumors, bronchiectasis, and pleural pathology.
PULMONARY FUNCTION TEST:-FEV1, FVC, FEV1/FVC PEFR.
BLOOD GAS ANALYSIS:
BRONCHOSCOPY: fiberoptic bronchoscopy.
rigid bronchoscopy.
SWEAT CHLORIDE TEST: <40 mEq/L normal.
>60 mEq/L in Cystic fibrosis.
TREATMENT
REACTIVE AIRWAY DISEASE:
 1)Asthaline Nebulization A:NS (0.25:2.5 ml)
1)Asthaline Nebulization A:NS (0.25:2.5 ml)
2)Antibiotics if superadded infection.
BRONCHIOLITIS:
- O2 inhalation.
- Ribavirin.
- Adrenaline.
ASTHMA:
- Bronchodilators: salbutamol, terbutaline
- Corticosteroids: Beclomethasone,
- Fluticasone
- Mast cell stabilizers: sodium cromoglycate.
- Ketotifen.
- leukotriene modifiers: Montelukast ,
- Zafirlukast
- Immunotherapy
FOREIGN BODY ASPIRATION:
Bronchoscopy.
CYSTIC FIBROSIS:
- Postural drainge.
- chest clamping.
- mucolytic agent.
- antibiotic therapy( fluroquinolones)
- Bronchodilators and inhalation of
- steroids
- Nutritional Management.




2 Comments
nice article
Thanks Dr. saurav, for nice article.
Comments are closed.