Ketone bodies, Ketosis and Ketoacidosis
Ketone bodies, produced mainly in the mitochondria of liver cells from acetyl-CoA enter blood, provide much of the energy to heart tissue, and during starvation to the brain. They include 3 water soluble chemicals namely: acetone, acetoacetate and β-hydroxybutyrate (not a true ketone). The levels of acetone are much lower than those of the other 2 ketone bodies; it cannot be converted back to acetyl-CoA and so is excreted in the urine or breathed out.
In the liver, ketone bodies are synthesized in the mitochondrial matrix from acetyl-CoA generated from fatty oxidation and this process is known as ketogenesis. Acetyl-CoA results from the breakdown of carbohydrates, lipids and certain amino acids. Normally, the acetyl group of acetyl-CoA enters the citric acid cycle to generate energy in the form of ATP, but it can also form ketone bodies; this happens if acetyl-CoA levels are high and the TCA cycle capacity is exceeded (the limiting factor is the availability of oxaloacetate).
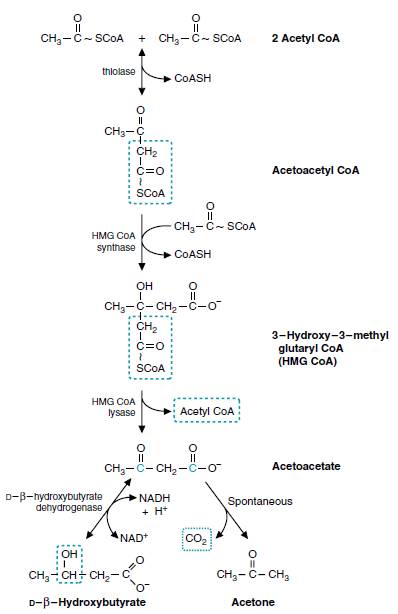
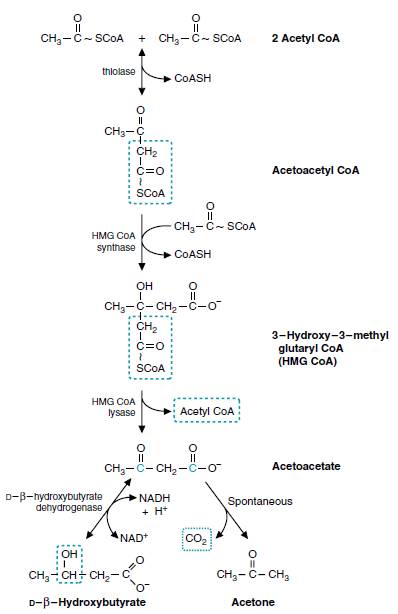
Steps in ketogenesis:
- Catalyzed by enzyme thiolase, 2 molecules of acetyl-CoA condense to form acatoacetyl-CoA.
- Catalyzed by enzyme HMG-CoA synthase, acetoacetyl-CoA combines with another molecule of acetyl-CoA to produce HMG-CoA (β-hydroxy β-methyl glutaryl-CoA).
- HMG-CoA lyase cleaves HMG-CoA to produce acetoacetate and acetyl-CoA.
- Acetoacetate can undergo spontaneous decarboxylation to form acetone.
- Acetoacetate can be reduced by a dehydrogenase to β-hydroxybutyrate.
The dehydrogenase reaction is readily reversible and interconverts the 2 ketone bodies, which exist in an equilibrium ratio determined by NADH/NAD+ ratio of the mitochondrial matrix. Under normal conditions, the ratio of the 2 ketone bodies in the blood is approxiamtely 1:1.
Regulation:
When fat enters liver it has 2 fates: either
- Beta oxidation (Occurs during glucose deficiency)
- Storage as triacylglycerol (Occurs when liver has sufficient supplies of glycerol 3 phosphate from glycolysis)
Hormones:
- Hunger stimulates Glucagon hormone responsible for stimulating Fatty acid oxidation and Ketogenesis
- Fed state stimulates Insulin hormone responsible for inhibiting ketogenesis
How are Ketone Bodies utilized?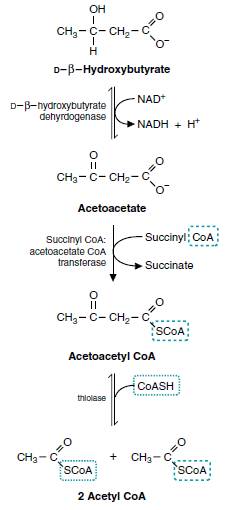
The ketone bodies being water soluble, are easily transported from the liver to various tissues. Acetoacetate and β-hydroxybutyrate can be oxidized as fuels in most tissues includin skeletal muscle, brain, certain cells of kidney and cells of the intestinal mucosa. The tissues which lack mitochondria (eg. erythrocytes) cannot utilize ketone bodies. During prolonged starvation, ketone bodies are the major sources of fuel for the brain and other parts of central nervous system (CNS).
Steps in oxidation of ketone bodies (ketogenolysis):
- β-hydroxybutyrate is converted back to acetoacetate.
- Acetoacetate is activated to Acetoacetyl-CoA by a mitochondrial enzyme thiophorase (succinyl-CoA : acetoacetate-CoA transferase). Thiophorase is absent in liver, hence ketone bodies are not utilized in the liver.
- Thiolase cleaves acetoacetyl-CoA to 2 moles of acetyl-CoA
- The principal fate of the acetyl-CoA synthesized is the oxidation in TCA cycle.
Ketosis:
The concentration of ketone bodies in blood is maintained around 1 mg/dl. The excretion in urine is very low and undtectable by routine tests (Rothera’s test).
When the rate of synthesis of ketone bodies exceeds the rate of utilization, their concentration in blood increases, this is known as ketonemia. This is followed by ketonuria – excretion of ketone bodies in urine. The overall picture of ketonemia and ketonuria is commonly referred to as ketosis. Smell of acetone in breathe is a common feature of ketosis. It is most commonly associated with following conditions:
Starvation: Starvation is accompanied by increased degradation of fatty acids to meet energy needs of the body. This causes an overproduction of acetyl-CoA which cannot be entirely handled by TCA or citric acid cycle. Furthermore, TCA cycle is impaired due to deficiency of oxaloacetate, since most of it is diverted for glucose synthesis (gluconeogenesis) to meet the essential requirements (often unsuccessful) for tissues like brain. The result is an accumulation of acetyl-CoA and overproduction of ketone bodies leading to ketosis.
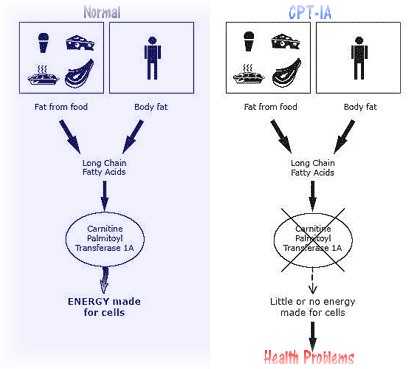
Diabetes Mellitus type I (Insulin Dependent):
- Hyperglycaemia occurs due to decreased glucose uptake in fat and muscle cells due to insulin deficiency
- Lipolysis in fat cells now occurs promoted by the insulin deficiency releasing Free fatty acids (FFA) into the blood which provide substrate to the liver
- A switch in hepatic lipid metabolism occurs due to the insulin deficiency and the glucagon excess, so the excess FFA is metabolised resulting in excess production of acetyl CoA
- The excess hepatic acetyl CoA (remaining after saturation of TCA cycle) is converted to ketone bodies which are released into the blood
- Ketoacidosis and hyperglycaemia both occur due to the lack of insulin and the increase in glucagon and most of the clinical effects follow from these two factors