Acute Liver failure: Classification, causes, features and management
Also Known as Fulminant Hepatic Failure, it is a Syndrome in which hepatic encephalopathy, characterized by mental changes progressing from confusion to stupor and coma, and results from a sudden severe impairment of hepatic function. According to some authors, Acute liver failure is a broad term and encompasses both fulminant hepatic failure and sub fulminant hepatic failure.
Fulminant hepatic failure (FHF) which is defined as the severe impairment of hepatic functions or severe necrosis of hepatocytes in the absence of preexisting liver disease ( encephalopathy within 8 weeks of the onset of symptoms in a previously healthy liver).
Defined originally further as-
- occurring within 8 weeks of onset of precipitating illness.
- In the absence of evidence of pre-existing liver disease
Classified as-
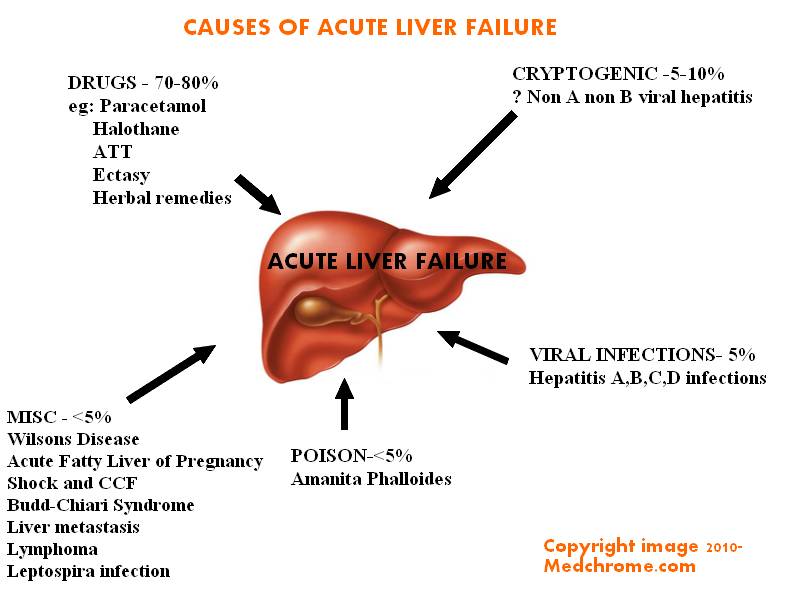
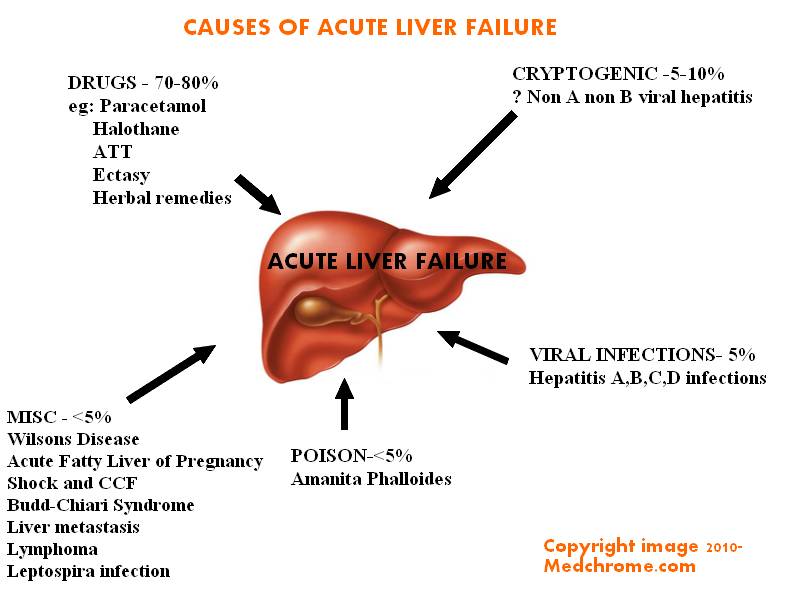
- Hyperacute – occurring in less than 7 days. Cerebral edema is common. Commonly caused by viral hepatitis and paracetamol poisoning .
- Acute- Occurring between 1 week to 4 weeks. Cerebral edema is common. Follows Drug toxicity and cryptogenic causes.
- Sub-acute- Occurring between 4 weeks to 12 weeks. Cerebral edema is uncommon. Cryptogenic causes and drugs are main causes.
Clinical Assessment-
- Mild episodic symptoms may progress up to hepatic encephalopathy later causing severe cerebral disturbances.
- Reduced alertness, poor concentration
- Behavioural changes- aggressive and restless.
- Altered sensorium
- Flapping tremor or Asterexis
- Fetor hepaticus ( typical smell breath in liver disease)
- Abnormal pupillary reaction
- Hypertension, Bradycardia, hyperventilation
- Profuse sweating, Myoclonus, focal fits, decerebrate posturing and late- Papilloedema
General Symptoms are-
Weakness, nausea and vomiting, right hypochondrial discomfort
Examination may reveal-Jaundice, Reye’s Syndrome
- Fetor hepaticus
- Hepatomegaly is unusual
- Sudden onset ascites
- Normal spleen size
Investigation useful for assessing the problem are-
- Toxicology Screen of blood and urine for drugs and toxins
- Hepatitis Virus Antibody screening and test to detect CMV, EBV, HSV etc
- Liver function test
- Serum Caeruloplasmin level, Serum copper, Urinary copper, Slit lamp eye examination to rule out Wilson’s Disease
- Auto-antibodies like ANF, ASMA, LKM
- Ultrasonography – Liver and Doppler of Hepatic veins
Management-
- Patient is critical and need ICU care
- Monitor – Neurological, Cardiorespiratory functions
- Fluid balance- maintenance and input/output charting
- Blood Analysis- Arterial Blood Gas Analysis, Peripheral blood count, Electrolytes,Glucose-2 hourly
- Kidney function test
- Prothrombin time
- Infection Survillence-
- Culture Blood, urie throat, sputum, cannula sites
- Chest x-ray
Treatment-
- Conservative treatment is Dialysis for removal of toxins and drugs
- Paracetamol Poisoning-NAC (Read Paracetamol poisoning in children)
- Liver transplant
Monitor the adverse prognostic criteria.
Complications – ( HERMIM – Mnemonic)
- Hypoglycemia
- Encephalopathy and cerebral edema
- Renal failure
- Metabolic acidosis
- Infection
- MODS
Survival – 1 yr =60%