Malignant Hyperthermia (MH): Clinical features, Diagnosis, Management
Definition: A hypermetabolic state that occurs in genetically susceptible patients on exposure to a triggering agent.
Triggering agents:
- Suxamethonium or Succinylcholine (Depolarizing skeletal muscle relaxant)
- All anesthetic volatile agents (eg. halothane)
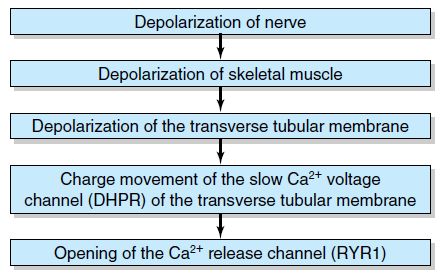
Biochemical basis:
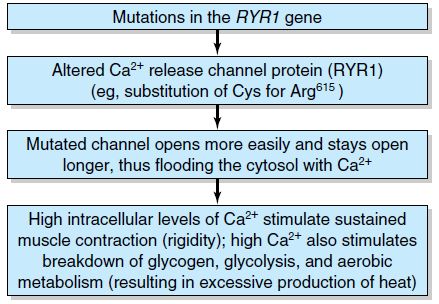
It is inherited as an autosomal dominant condition and caused by loss of normal Ca2+ homeostasis at some point along the excitation-contraction coupling process on exposure to triggering agents. Most likely site is the triadic junction between T tubule, involving the voltage sensor of the dihydropyridine receptor (DHPR), and sarcoplasmic reticulum (SR), involving the Ca2+ efflux channel of the ryanodine receptor (RYR1). About 60% of Malignant Hyperthermia families are linked to the RYR1 gene located on chromosome 19q.
Clinical features:
- Core temperature increases by 2 degree celsius per hour or more, or 0.5 degree celsius every 15 minutes.
- On exposure to a triggering agent patients undergo a sustained muscular contraction.
- Failure to relax after suxamethonium.
- The 1st sign may be masseter muscle spasm or inability to open the mouth after giving suxamethonium; however not all masseter spasms progress to malignant hyperthermia.
- Tachycardia, cardiac arrhythmias and cardiovascular collapse.
- Increased end-tidal carbon dioxide (ETCO2) and tachypnea if the patient is breathing spontaneously.
- Metabolic and respiratory acidosis.
- Generalized muscular rigidity.
- Hyperkalemia.
- Myoglobinurea causing acute tubular necrosis.
- Previously uneventful general anesthesia or exposure to triggers does not rule out the diagnosis.
- Signs of increased metabolism: tachycardia, dysrhythmias, increased CO2 production, metabolic acidosis, pyrexia, DIC
- Muscle signs: masseter spasm after suxamethonium, generalized muscle rigidity, hyperkalemia, high CK, myoglobinuria, renal failure
The Differential diagnoses for masseter muscles spasm (MMS) are:
- Myotonic syndrome
- TMJ dysfunction
- Underdosing with suxamethonium
- Not allowing sufficient time for suxamethonium to act before intubation
- Increased muscle tone after suxamethonium in the presence of fever or elevated plasma catecholamine
Risk factors:
- Positive family history
- History of malignant neuroleptic syndrome
- Muscular dystrophy
- Trismus on induction (jaw rigidity)
- Arthrogryposis multiplex congenita, osteogenesis imperfecta, ongenital strabismus, central core disease
Diagnosis:
- A small piece of striated muscle biopsied from the patient is challenged in vitro with a triggering agent (halothane or caffeine).
Differential Diagnosis:
- Inadequate anesthesia or analgesia
- Inapprropriate breathing circuit/fresh gas flow/ventilation
- Endocrine disorders: Pheochromocytoma, Thyrotoxicosis
- Sepsis
- Hypoxic encephalopathy
- Other muscle disorders
Action:
- Discontinue the triggering agent and end surgery if possible.
- Give 100% oxygen.
- Change the anesthetic machine to a vapour-free machine.
- Maintain anesthesia with an alternative agent e.g. propofol.
- Dantrolene 1-2 mg/kg i.v. should be given and repeated every 5 min, until the temperature and CO2 stop rising, upto a total of 10 mg/kg.
- Treat acidosis with sodium bicarbonate 8.4%.
- Treat hyperkalemia with insulin and glucose.
- Lower temperature by:
- Body surface cooling
- Cooling blankets
- Cool irrigation fluids
- Extracorporeal cooling may be indicated.
- Maintain urine output >1 ml/kg/h.
- Admit the patient to ICU for supportive therapy, prevention of secondary complications and close monitoring for recurrence.
- Arrange muscle biopsy testing of patient (and near relatives if diagnosis confirmed).
Anesthesia in patients with Malignant hyperthermia susceptibility:
- Ensure dantrolene is available.
- Use a vapour-free anesthetic machine, flushed with 100% oxygen for 5 minutes at a fresh gass flow rate of 10 litres/minute.
- All circuits should be disposable and new.
- The soda lime should be previously unused.
- Regional anesthesia is safe.
- Drugs which are considered safe include barbiturates, narcotics, nitrous oxide, propofol, benzodiazepines, non-depolarizing muscular blocking agents.
- A total intravenous technique using propofol along with an infusion of short acting opioids is safest.
Source:
- Churchill’s Pocketbooks Anaesthesia – Nathanson and Mahajan
- Oxford Handbook of Anaesthesia – 2nd edition