Pyogenic Liver Abscess

Liver Blood supply:
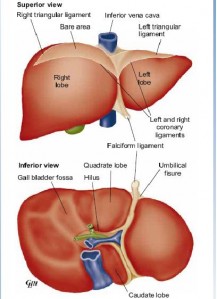
The liver derives blood from the hepatic artery (20%) and the portal vein (80%).
The hepatic artery usually arises from the aorta at the coeliac axis and divides into the right and left branches at the hilus.
The venous drainage from the liver is by three large hepatic veins right, middle and left into the inferior vena cava (IVC), just below the diaphragm.
The 3 major forms of liver abscess,
classified by etiology, are as follows:
1. Pyogenic abscess, which is most often polymicrobial, accounts for 80% of hepatic abscess cases in the United States.
2. Amebic abscess due to Entamoeba histolytica accounts for 10% of cases.
3. Fungal abscess, most often due to Candida species, accounts for less than 10% of cases.
Risk factors : DM, underlying hepatobiliary or pancreatic malignancy, and liver transplant. Geographic factors may also play a role. mortality rate : 2 ~ 12% (mortality appears to be related to underlying comorbidities rather than to the abscess itself.)
Pathophysiology:
The liver receives blood from both systemic and portal circulations. Increased susceptibility to infections would be expected given the increased exposure to bacteria. However, Kupffer cells lining the hepatic sinusoids clear bacteria so efficiently that infection rarely occurs. Multiple processes have been associated with the development of hepatic abscesses
Causes:
Infection through portal vein:
acute appendicitis, diverticulitis, amoebic colitis, UC
Infection through the CBD:
stricture, periampullary Ca, rec. cholangitis, ERCP
Infection through hepatic artery:
septicemia, pyaemia
Extension abscess:
sudiaphragmatic abscess, empyema thoracis, injuries
Infection through umbilicus:
neonatal umbilical sepsis giving rise to pyaemia
Pyogenic liver abscess has been reported as a secondary infection of
- 1.amebic abscess
- 2.hydatid cystic cavities and metastatic and primary hepatic tumors.
- 3.complication of liver transplantation
- 4.hepatic artery embolization in the treatment of hepatocellular carcinoma
- 5.ingestion of foreign bodies, which penetrate the liver parenchyma.
- Appendicitis was traditionally the major cause of liver abscess. Biliary tract disease is now the most common source of pyogenic liver abscess.
- Abscesses usually are multiple, unless they are associated with surgical interventions or indwelling biliary stents. In these instances, solitary lesions can be seen.
- The right hepatic lobe is affected more often than the left hepatic lobe by a factor of 2:1. Bilateral involvement is seen in 5% of cases. The predilection for the right hepatic lobe can be attributed to anatomic considerations. The right hepatic lobe receives blood from both the superior mesenteric and portal veins, whereas the left hepatic lobe receives inferior mesenteric and splenic drainage. It also contains a denser network of biliary canaliculi and, overall, accounts for more hepatic mass. Studies have suggested that a streaming effect in the portal circulation is causative.
Symptoms:
The most frequent symptoms of hepatic abscess include the following:
- Fever (either continuous or spiking)
- Chills
- Right upper quadrant pain
- Anorexia
- Malaise
- Cough or hiccoughs due to diaphragmatic irritation may be reported.
- Referred pain to the right shoulder may be present.
- Individuals with solitary lesions usually have a more insidious course with weight loss and anemia of chronic disease. With such symptoms, malignancy often is the initial consideration.
- Fever of unknown origin (FUO) frequently can be an initial diagnosis in indolent cases.
- Afebrile presentations have been documented.
Physical Signs:
- Fever and tender hepatomegaly -the most common signs.
- A palpable mass need not be present.
- Mid epigastric tenderness, with or without a palpable mass, is suggestive of left hepatic lobe involvement.
- Decreased breath sounds in the right basilar lung zones, with signs of atelectasis and effusion on examination or radiologically, may be present.
- A pleural or hepatic friction rub can be associated with diaphragmatic irritation or inflammation of Glisson capsule.
- Jaundice may be present in as many as 25% of cases and usually is associated with biliary tract disease or the presence of multiple abscesses
Differential Diagnosis of Hepatic Abscess:
1.Biliary Disease 2. Hydatid Cysts 3.Cholecystitis 4. Pneumonia, Bacterial 5.Empyema, Pleuropulmonary 6.Gastritis, Acute 7.Hepatocellular Carcinoma
Lab Investigations:
- CBC count with differential ¡Anemia of chronic disease
- Neutrophilic leukocytosis Liver function studies
- Hypoalbuminemia and elevation of alkaline phosphatase (most common abnormalities)
- Elevations of transaminase and bilirubin levels (variable) Blood cultures are positive in roughly 50% of cases.
- Culture of abscess fluid should be the goal in establishing microbiologic diagnosis. ELISA for E. histolytica
- CT and ultrasound – modalities of choice Abscesses must be distinguished from tumors and cysts. CT or ultrasound-guided aspiration should be sent for gram stain and culture. Blood cultures should always be performed when liver abscess is suspected; they are positive in up to 50 percent of cases
Complications:
Sepsis Empyema resulting from contiguous spread or intrapleural rupture of abscess Rupture of abscess with resulting peritonitis Endophthalmitis when an abscess is associated with K pneumoniae bacteremia
MANAGEMENT of LIVER ABSCESS:
Percutaneous needle aspiration Under CT scan or ultrasound guidance, needle aspiration of cavity material can be performed. Diagnostic + therapeutic.
Percutaneous drainage has become the standard of care and should be the first intervention considered for small cysts. Seldinger or trochar technique.
For single abscesses with diameter ≤5 cm : percutaneous catheter drainage or needle aspiration is acceptable. For single abscesses with diameter >5 cm :percutaneous management : catheter drainage is preferred over needle aspiration. ¡surgical intervention is preferred over percutaneous drainage
Medical Therapy
- Empiric broad-spectrum antibiotics should be administered pending abscess gram stain and culture results.
- A third generation cephalosporin such as ceftriaxone PLUS metronidazole.(Flumarin)
- fluoroquinolone (eg, ciprofloxacin PLUS metronidazole
- Monotherapy with a carbapenem
follow imaging, WBC count and serum CRP If good response – 2~4 weeks of therapy, no or incomplete drainage- 4~6 weeks of therapy. Drainage catheters should remain in place until drainage is minimal (usually up to seven days).
Open surgery can be performed by 2 approaches.

- A transperitoneal approach allows for abscess drainage and abdominal exploration to identify previously undetected abscesses and the location of an etiologic source.
- For high posterior lesions, a posterior transpleural approach can be used.
- A laparoscopic approach is also commonly used in select cases.
( Source Medscape-emedicine, Manipal, Bailey and Love and various sites).