Definition: Inflammation of the pancreas due to parenchymal autodigestion by proteolytic enzymes
The clinical definition of acute pancreatitis, whether in the presence or absence of underlying chronic pancreatitis, requires atleast 2 of the following 3 features:
- Clinical assessment: Abdominal pain suggestive strongly of acute pancreatitis.
- Enzymes: Serum amylase and/or lipase activity at least 3 times greater than the upper limit of normal.
- Imaging: Characteristic findings of acute pancreatitis on transabdominal ultrasonography or on CECT.
ETIOLOGY: GET SMASHED
- G: Gall stones (60%) *
- E: Ethanol (30%) *
- T: Trauma *
- S: Surgical (Post-operative*), Scorpion sting
- M: Mumps and Coxsackie infection, Mysterious (Idiopathic *)
- A: Autoimmune (Polyarteritis Nodosa)
- S: SPINK-1, PRSS1 mutation (Genetic)
- H: Hypertriglyceridemia *, Hypocalcemia, Hypothermia
- E: ERCP *
- D: Drugs *(Corticosteroids, Thiazides, Valproate, Azathioprine, Estrogen, Sulfonamides, Tetracycline, 6-Mercaptopurine, anti-HIV medications)
Common causes are indicated with *
Drugs causing pancreatitis: SAVED IMP
- S: Sulindac, Sulfonamides
- A: Azathiporine, Acetaminophen
- V: Valproate
- E: Estrogen
- D: Diuretics, Dideoxynosine
- I: Isoniazid
- M: Metronidazole, Methyldopa
- P: Phenytoin, Procainamide
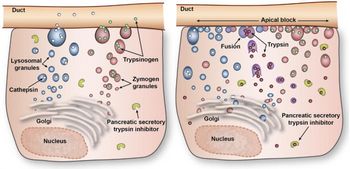
PATHOPHYSIOLOGY
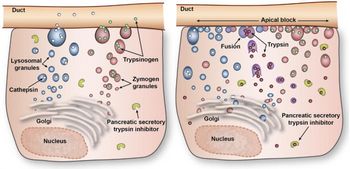
A) 1st Phase: Premature activation of trypsin within pancreatic acinar cell leading to activation of varieties of injurious pancreatic enzymes. Proposed mechanisms:
- Disruption of calcium signalling in acinar cells
- Cleavage of trypsinogen to trypsin by lysosomal hydrolase cathepsin-B which becomes co-localized with digestive enzymes in intracellular organelles (Co-localization theory)
- Decreased activity of intracellular pancreatic trypsin inhibitor
B) 2nd Phase: Intrapancreatic inflammation
C) 3rd Phase: Extrapancreatic inflammation including ARDS
Pathology:
Acute pancreatitis is a group of reversible lesions characterized by inflammation of pancreas ranging in severity from edema and fat necrosis to parenchymal necrosis with severe hemorrhage.
- Acute interstitial inflammation and edema –> Swollen and edematous pancreas
- Protease –> Liquefactive necrosis of pancreatic parenchyma –> Grey-white liquefactive necrosis
- Lipase, Phospholipase –> Fat necrosis –> foci of yellow white chalky fat necrosis
- Elastase –>Interstitial hemorrhage due to blood vessel destruction –> Areas of red-black hemorrhage
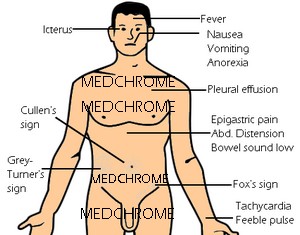
CLINICAL FEATURES
Symptoms: Abdominal pain (LIQOR AAA)
- Location: Upper abdomen/Epigastric
- Length (Duration): More than a day
- Intensity: Gradually becomes severe
- Quality: Constant and Dull
- Onset: Sudden
- Radiation: Back
- Associated symptoms: Nausea, Vomiting, Anorexia, Abdominal distension
- Aggravating factors: Eating or drinking (specially alcohol)
- Alleviating factors: Leaning forward, Curl up (Fetal position)
Epidemiology:
- Age: Young/middle age
- Sex: Males (Commonly alcohol related) > Females (Commonly biliary tract disease related)
- General condition: Distressed, Anxious
- Vitals: Fever (~75%), Tachycardia (~65%), Hypotension, Tachypnea
- Cardinals: Jaundice (~30%), Cyanosis, Dehydration
- Respiratory: Signs of pleural effusion – usually left sided (sometimes)
- Abdominal: Marked epigastric tenderness with voluntary and involuntary guarding (~70%) +/- rigidity, Abdominal distension (~65%), Reduced bowel sound, Palpable pseudocyst (sometimes)
- Uncommon signs associated with severe necrotizing pancreatitis:
- Cullen’s sign (Periumbilical discoloration due to peritoneal hemorrhage)
- Grey-Turner’s sign (Flank discoloration due to retroperitoneal hemorrhage)
- Fox’s sign (Discoloration below inguinal ligament or at the base of penis)
- Erythematous skin nodules (Subcutaneous fat necrosis)
Mechanism of signs:
- Abdominal distension and Decreased bowel sound: Paralytic ileus (Peripancreatic spread of inflammation)
- Jaundice: Choledochal obstruction due to gallstone or edema of pancreatic head
- Tachycardia, hypotension, dehydration: Hypovolemia due to sequestration of fluid in pancreatic bed (3rd space loss)
- Fever: Peripancreatic inflammation
- Tachypnea: Diaphragmatic inflammation, Pleural effusion, ARDS
- Cyanosis: ARDS
DIFFERENTIAL DIAGNOSIS
1. Mesenteric ischemia or infarction
2. Perforated peptic ulcer
3. Biliary colic
4. Renal colic
5. Dissecting aortic aneurysm
6. Myocardial infarction
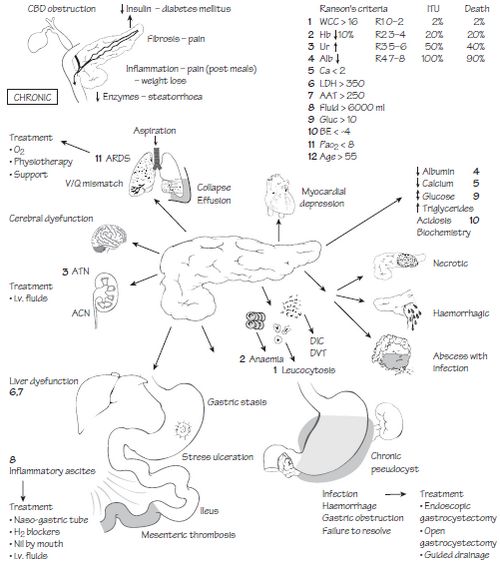
COMPLICATIONS
Local:
- Necrosis:
- Sterile
- Infected
- Pancreatic fluid collections:
- Pancreatic abscess
- Pancreatic pseudocyst (Pain, rupture, hemorrhage, infection, obstruction of GIT)
- Pancreatic pseudoaneurysm (Erosion of adjacent artery by pseudocyst)
- Pancreatic ascites
- Disruption of main pancreatic duct
- Leaking pseudocyst
- Involvement of contiguous organs by necrotizing pancreatitis
- Massive intraperitoneal hemorrhage
- Thrombosis of blood vessels (splenic vein i.e. sinistral portal HTN, portal vein)
- Bowel obstruction
- Obstructive Jaundice
Systemic:
- Pulmonary: Pleural effusion, Atelectasis, Mediastinal abscess, Pneumonitis, ARDS
- Cardiovascular: Hypotension (Hypovolemia), Sudden death, Pericardial effusion
- Hematologic: Disseminated Intravascular Coagulation (DIC)
- Gastrointestinal hemorrhage: Peptic ulcer disease, Erosive gastritis, Hemorrhagic pancreatic necrosis with erosion into major blood vessels, Portal vein thrombosis (Variceal hemorrhages)
- Renal: Oliguria, Azotemia, Renal artery/vein thrombosis, Acute Tubular Necrosis
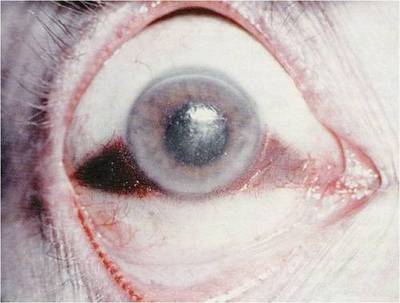
- Metabolic: Hyperglycemia, Hypocalcemia, Encephalopathy, Sudden blindness (Purtscher’s retinopathy)
- CNS: Psychosis, Fat emboli
Timeline of Complications:
- Week 1: Pain, Fluid electrolyte imbalance, Metabolic disturbance, Multiorgan failure due to SIRS
- Week 2-6: Infection of Pancreatic necrosis, Fluid collections
- > 6 weeks: Pseudocyst formation
SIRS (Systemic Inflammatory Response Syndrome) is defined by > or = 2 criteria:
- Pulse >90 beats/min
- Respiratory rate >20/min or PCO2 <32 mmHg
- Rectal temperature <36◦C or >38◦C
- White blood count <4,000 or >12,000/mm3
INVESTIGATIONS AND DIAGNOSIS
Laboratory studies:
- Serum amylase and lipase: ↑ by 3X of upper-limit is diagnostic
- LFTs: ↑ ALT and AST (ALT ↑ by around 3X i.e. >150 IU/L is diagnostic of gall stone pancreatitis), ↑ALP, ↑bilirubin, ↓albumin
- RFTs: BUN and Creatinine (to rule out renal failure)
- CBC and HCt: Leukocytosis with shift to left (Inflammation or SIRS), ↑HCt (Hemoconcentration due to fluid sequestration), ↓HCt (Dehydration or Hemorrhage)
- Blood biochemistry:
- Blood sugar: may ↑ due to insulin producing Beta-cell dysfunction
- Serum calcium: ↓ (due to hypoalbuminemia or fat necrosis) or ↑ (if hypercalcemia is etiology)
- Lipid profile: to rule out hypertriglyceridemia as the cause
- ABG: every 12 hrs for 1st 3 days (to monitor oxygenation and acid-base status)
- Other: CRP, Trypsin, Trypsinogen-2, LDH, Phospholipase A
Note:
- Lipase is more specific than amylase (hence preferred)
- Other causes of ↑ amylase: Macroamylasemia, Renal failure, Mumps parotitis, ERCP induced, Esophageal perforation, Pregnancy
Imaging studies:
1. Plain CXR: To detect pleural effusion, ARDS (Basal atelectasis and infiltrates), Elevation of left diaphragm
2. Plain AXR (erect):
- To rule out perforated peptic ulcer
- Sentinel loop sign: Dilated proximal jejunal loop adjacent to pancreas because of local ileus
- Colon ‘cut-off’ sign: Distended transverse colon with collapsed descending colon
- May show gallstone, pancreatic calcification
3. Abdominal USG: Can detect gallstones, biliary obstruction, pseudocyst formation
4. CT abdomen: may be required if diagnosis uncertain, to rule out and find degree of:
- Peripancreatic collection
- Necrosis
- Abscess
5. MRCP, ERCP, EUS: indicated in patients with elevated LFTs suggestive of bile duct obstruction to exclude strictures, neoplasms or stones
Abbreviations used:
LFT (Liver Function Test), RFT (Renal Function Test), CBC (Complete Blood Count), HCt (Hematocrit), ABG (Arterial Blood Gas), CRP (C-reactive Protein), CXR (Chest X-ray), AXR (Abdominal X-ray), USG (Ultrasonography), CT (Computed Tomography), MRCP (Magnetic Resonance Cholangiopancreatography), ERCP (Endoscopic retrograde Cholangiopancreatography), EUS (Endoscopic Ultrasound), MC+S (Microscopy, Culture, Sensitivity)
Summary of Investigations:
- Bloods: CBC, HCt, Ca2+, LFT, CRP, Amylase, Lipase, LDH, Glucose
- Urinanalysis: Dipstick , Urinalysis MC+S
- Radiology: Erect CXR, AXR, USG, CT
- Other: ABG
SEVERITY PREDICTION
A) Ranson’s criteria: Non-Biliary (N) vs Biliary (B)
On Admission: ABCDE
- Age > 55 yrs (N) vs > 70 yrs (B)
- Blood cell (WBC) > 16,000/ml (N) vs 18,000/ml (B)
- Carbohydrate (Glucose) > 200 mg/dl (N) vs >220 mg/dl (B)
- Diagnostic Enzymes:
- AST > 250 IU/L (N and B)
- LDH > 350 IU/L (N) vs >400 IU/L (B)
Within initial 48 hrs: ABCDEF
- ABG (PaO2) < 60 mmHg (N and B)
- ↑BUN > 5 mg/dl (N) vs > 2mg/dl (B)
- Ca2+ < 8 mg/dl (N and B)
- DEficit:
- Base deficit > 4 mEq/L (N) vs > 5 mEq/L (B)
- Fluid deficit > 6L (N) vs >4L (B)
- Fall in HCt > 10%
Mortality risk by Ranson criteria:
- R1 (0-2): 1%
- R2 (3-4): 16%
- R3 (4-6): 40%
- R4 (>6): near 100%
Calculating Total Body Water Deficit (TBWD):
- TBWD males = [(140 – Serum Na+) X 0.6 X Body wt. in kg]/140
- TBWD females = [(140 – Serum Na+) X 0.5 X Body wt. in kg]/140
B) APACHE-II score (Acute Physiology and Chronic Health Evaluation)
Scoring parameters:
- Physiological: Temperature, Heart rate, Respiratory rate, Mean Arterial Pressure, Glasgow Coma Scale
- Laboratory: PaO2, pH, serum Na, K, creatinine, Hematocrit, WBC count
Mortality risk by APACHE-II score:
- <8: 4%
- >8: 10-20%
C) Severe Acute Pancreatitis Criteria by Atlanta Symposium
1. Early Prognostic signs:
- Ranson signs > or = 3
- APACHE-II score > or = 8
2. Organ failure:
- Cardiovascular: Shock i.e. Systolic BP < 90mmHg
- Pulmonary: PaO2 < or = 60mmHg
- Renal: Creatinine > 2mg/L after rehydration
- Gastrointestinal: GI bleeding > 500ml/24hr
And/Or
3. Local complications:
- Necrosis
- Abscess
- Pseudocyst
Other factors indicating severe disease:
- Obesity (BMI > 29)
- Hemoconcentration (HCt > 44%)
- CRP > 150 mg/L
MANAGEMENT
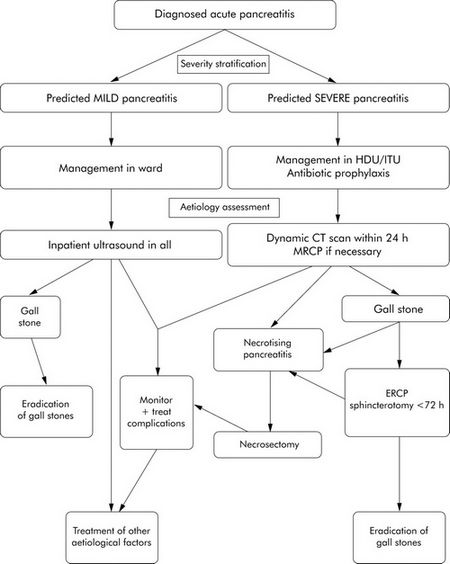
A) Hospitalization: Admission in ward if predicted mild pancreatitis and in ICU if predicted severe pancreatitis
B) General supportive treatment: To prevent complications
- NPO + IV fluids
- Oxygen as necessary
- IV Analgesics (Morphine shouldn’t be used as it increases sphincter of oddi pressure and may exacerbate pancreatitis)
- No proven use for routine Nasogastric tube or Antibiotics
- NG tubes indicated for: Severe ileus (AXR), Severe abdominal distension (PE) or Persistent emesis
- Prophylactic antibiotics indicated for: Severe pancreatitis (Better to discontinue if blood and other cultures or negative for infection) – Antibiotics used must be bactericidal (imipenem, 3rd generation cephalosporins, metronidazole, etc.)
- Frequent measurement of adequacy of fluid resuscitation: Vital signs, Urine output, Decrease of HCt
- If the disease is severe: Transfer to ICU and invasive monitoring (Central catheter for CVP or Swan-Ganz catheter)
- Stepwise nutrition as condition improves:
- In Mild disease: Oral feeding is usually restored within 3-7 days and nutritional support is not needed. The diet is initially clear fluid, low in fat and small in amount which is adjusted gradually as tolerated by patient.
- In Severe disease: Patient usually cannot be restored to oral feeding due to persistent signs and symptoms. So nutritional support is required i.e. enteral or parenteral nutrition (peripheral or TPN)
Enteral nutrition is preferred over TPN:
- In severe acute pancreatitis gut barrier function is compromised resulting in increased intestinal permeability to bacteria and endotoxins. Enteral nutrition stabilizes gut barrier function and contributes to prevention of septic complications.
- Numerous complications of TPN (line sepsis, local abscess, pneumothorax, venous thromboembolism) can be avoided by using enteral feeding
- Stimulation of pancreatic secretion by the presence of food in the gut only pertains to food within the gastric or duodenal lumen. Nasojejunal feeding therefore does not stimulate exocrine pancreatic secretion and does not reactivate the pancreatitis.
C) Directed therapy for Specific causes:
1. Gallstone (Biliary) Pancreatitis:
- Mild pancreatitis: Laparoscopic cholecystectomy + Therapy for remaining CBD stone (Intreoperative/Postoperative ERCP or Laparoscopic or Open CBD exploration based on expertise)
- Severe pancreatitis/Cholangitis: Urgent ERCP and biliary sphincterotomy (preferably within 24 hrs) followed by gallstone eradication
2. Alcoholic Pancreatitis:
- Sedation and Vitamin supplements
D) Treatment of Complications:
- DIC: Cryoprecipitate, Fresh frozen plasma, RBC and platelet transfusion)
- ARDS: O2 + Continuous Positive Airway Pressure (CPAP)
- Renal insufficiency: Agressive IV hydration + Normolization of BP
- Infected pancreatic necrosis: Percutaneous drainage of pancreatic fluid + Antibiotics +/- Necrosectomy
- Pancreatic pseudocyst: Percutaneous drainage
- Ascites and Fistula: Stenting of pancreatic duct + Octreotide to decrease secretion or Surgery
- Splenic vein thrombosis: Thrombolysis + Splenectomy (If isolated gastric varices)
SOURCES:
-
Practice Guidelines in Acute Pancreatitis (Peter A. Banks, Martin L. Freeman), American Journal of Gastroenterology
-
Acute Pancreatitis: Etiology, Clinical Presentation, Diagnosis and Therapy (Mitchell S. Cappell)
-
Surgery At a Glance (Pierce A. Grace, Neil R. Borley)
-
Essential Revision Notes in Surgery For Medical Students (Irfan Halim)
-
Harrison’s Principle of Internal Medicine – 16th edition
-
Clinical Medicine – Kumar and Clarke 6th edition