A Review of Ectopic Pregnancy
Definition: Implantation and development of fertilized ovum outside the normal endometrial cavity
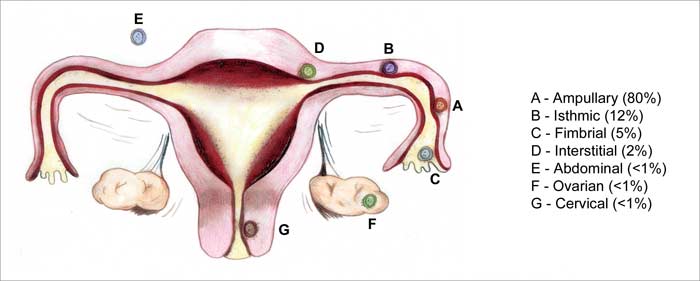
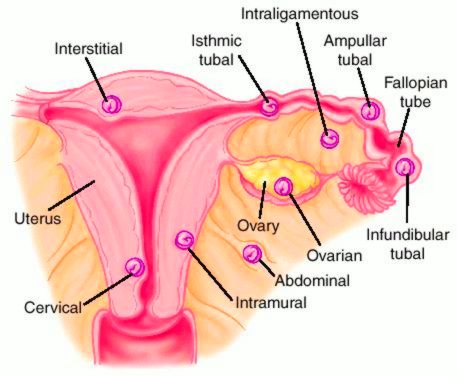
Sites of Implantation:
1. Extrauterine (98.5%):
- Tubal (97%): Ampulla, Isthmus, Indundibulum, Interstitium
- Ovarian (0.5%)
- Abdominal (1%): Secondary > Primary
2. Uterine (1.5%):
- Cervical (<1%)
- Angular
- Cornual (In bicornuate uterus)
- Cesarean section scar
Heterotopic pregnancy: combination of intrauterine and ectopic pregnancy.
Risk Factors:
- History of PID (Pelvic Inflammatory Disease)
- Tubal/Pelvic surgery
- Contraception failure
- Previous ectopic pregnancy
- History of infertility
- IUD (Intrauterine Contraceptive Device)
- Previous induced abortion
- Tubal endometriosis
The fertilized ovum requires ~ 6 days to migrate through the tube to the uterine cavity where it normally implants. Wherever the embryo finds itself at that time, it will begin to implant. So anything that causes a delay in transportation of the ovum will cause ectopic pregnancy i.e. damage to the cilia or obstruction of the Fallopian tubes.
TUBAL PREGNANCY
A) Modes of Termination
- Repeated small hemorrhage and partial absorption → Tubal mole → Complete absorption
- Intense tubal contraction → Tubal abortion → Pelvic hematocele or Diffuse intraperitoneal hemorrhage
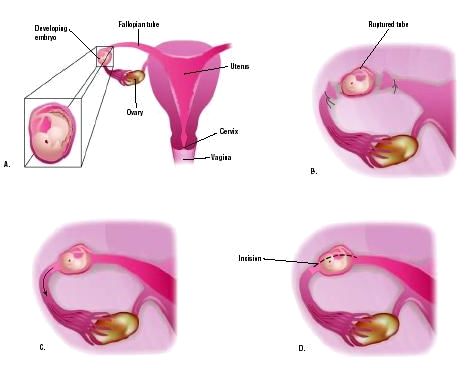
- Erosion of all layers of tube by chorionic villi → Tubal rupture → Diffuse intraperitoneal hemorrhage or Intraligamentary hematoma
- Tubal perforation → Secondary abdominal pregnancy or Intraligmanetary hemorrhage
B) Source of Vaginal bleeding:
Remember: It is not due to pelvic hematocele or intraperitoneal hemorrhage
Mechanism: Insufficient hCG → Corpus Luteum regress → Decreased progesterone → Endometrial support lost → Sloughing and bleeding
C) Clinical Features:
The clinical presentation usually depends upon the site of implantation in the tube:
- narrow part (isthmus or interstitium): rupture → acute presentation
- wider part (ampullae): abortion or absorption → subacute presentation or silent
Triad of: Abdominal pain (100%), Amenorrhea (75%) and Vaginal bleeding (70%)
1. Acute (Ruptured or Massive hemoperitoneum):
Symptoms:
- Severe abdominal pain
- Period of amenorrhea may not be appreciated due early rupture of tube
- Shoulder tip pain in 25% due to irritation of diaphragm (hemoperitoneum)
- Syncope (10%): dizziness and light-headedness
Signs:
- Ill looking, Pallor
- Shock: Rapid, feeble pulse, hypotension, cold clammy extremities
- Abdomen examination: Distended, tender, rebound tenderness, shifting dullness
- Pelvic examination: Cervical motion tenderness, Extreme tenderness on fornix palpation, Floating uterus, Blanched white vaginal mucosa, No mass felt
D/D of acute ectopic:
- Acute Appendicitis
- Ruptured CL
- Twisted ovarian tumor
- Ruptured chocolate cyst
- Perforated peptic ulcer
2. Unruptured:
- Bimanual examination: Pulsatile small, well circumscribed tender mass may be felt through one fornix separated from the uterus
- No features of Shock and collapse
3. Subacute (Chronic or Old):
Symptoms:
- Classic triad: Amenorrhea (6-10 weeks), Abdominal pain and Irregular vaginal bleeding
- Features of bladder irritation: Dysuria, frequency, retention
- Rectal tenesmus (Infected hematocele)
- Fever (Infection)
Signs:
- Ill looking, Pallor, High pulse, Elevated temperature
- No features of shock
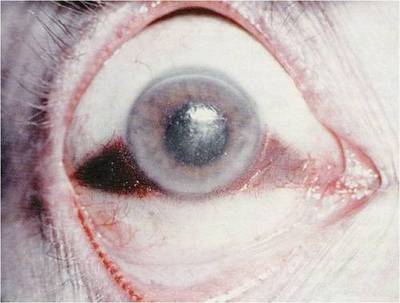
- Abdomen examination: Tenderness and muscle guarding, Mass in lower abdomen may be felt, Cullen’s sign (Periumbilical bluish discoloration – Intraperitoneal hemorrhage)
- Pelvic examination: Pale vaginal mucosa, Cervical motion tenderness, Ill defined/boggy adnexal mass
- Rectal examination
- Dilation and curettage (D&C): Arias-Stella phenomena i.e. proliferative, secretory and decidual reaction in histological examination.
D/D of subacute ectopic:
- Incomplete abortion
- Salpingitis
- Appendicitis
- Twisted ovarian tumor
- Ruptured chocolate cyst
- Ruptured CL
D) Investigations and Diagnosis
Blood: Hb, ABO, Rh, TLC, DLC, ESR
B-hCG (Urine pregnancy test):
- Lower concentration compared to normal intrauterine pregnancy
- Doubling time in plasma fails to occur in 2 days
Ultrasonoraphy (USG):
- Absence of intrauterine pregnancy with +ve pregnancy test
- Fluid in POD (Pouch of Douglas)
- Adnexal mass separated from ovary
Combination of B-hCG and USG:
- B-hCG must be >6000 IU/L (TAS) and >1500 IU/L (TVS) for gestational sac to be visible
- Empty uterine cavity with B-hCG >1500 IU/L (TVS) or >6000 IU/L (TAS)
- Failure to double B-hCG by 2 days along with empty uterus
TAS = Transabdmonial sonography and TVS = Transvaginal sonography
Serum Progesterone: Less than normal (<5ng/ml)
Culdocentesis (Rarely used):
- Withdrawal of > or = 5ml non-clotting blood from cul-de-sac (POD) through vagina
- Done to check for blood in POD but have high false –ve rate
Laparoscopy: Only when patient is hemodynamically stable
D+C: Decidua without villi
Laparotomy: When patient is hemodynamically unstable
In Acute ectopic: Only Hb estimation and Blood grouping (ABO, Rh)
F) Complications:
- Inevitable loss of fetus
- Hemorrhagic shock
- Future ectopic pregnancy
- Infertility
- Maternal death
- Rh sensitization
Practice recommendations
- Set a low threshold for suspicion of ectopic pregnancy. For any woman of childbearing age with abdominal pain and vaginal bleeding, consider pregnancy and take steps to rule out ectopic pregnancy.
- < 50% of the present with the classic triad given above.
- Definite cervical motion tenderness and peritoneal signs are the most sensitive and specific examination findings for ectopic pregnancy.
- β-hCG levels can be used in combination with ultrasound findings to improve the accuracy of the diagnosis of ectopic pregnancy.
- Women with initial nondiagnostic transvaginal ultrasound should be followed with serial β-hCGs.
E) Management
1. Acute Ectopic: Resuscitation and Laparotomy
Resusucitation:
- Ringer’s lactate (Crystalloids)
- Arrangement for Blood transfusion
- Volume replacement with colloids
Laparotomy:
- Salpingectomy
- Salpingectomy with Oophorectomy
- Subtotal hysterectomy (Interstitial pregnancy)
Tip: Don’t waste much time in resuscitation. Laparotomy must be proceeded immediately.
2. Chronic Ectopic:
- Elective laparotomy at earliest convenient time
- Salpingectomy
3. Unruptured Ectopic:
i. Expectant management:
Indications are:
- Initial B-hCG <1000 IU/L
- Falling hCG titre
- Ectopic mass diameter <4cm
- No evidence of bleeding or rupture
ii. Medical management:
Indications are:
- Hemodynamically stable
- Serum hCG <3000 IU/L
- Tubal diameter <4cm
- No fetal cardiac activity
- No intra-abdominal hemorrhage
a. Methotrexate (MTX): 50mg/m2 im
- Give folic acid after 30 hours
- Follow B-hCG levels on day 4 and 7
- If B-hCG level difference on day 4 and day 7 (D4-D7 ) > or = 15%: follow up weekly until hCG <10mIU/ml
- If D4-D7 < 15%: 2nd dose of MTX on Day 7
b. Others:
- KCl
- Prostaglandin (PGF2a)
- Hyperosmolar glucose
- Actinomycin
iii. Surgical management:
- Conservative
- Salpingostomy: Tube incised and only POC removed
- Segmental resection: Isthmic pregnancy
- Fimbrial expression (Milking): Ampullary pregnancy
- Extirpative
- Salpingectomy
Anti-D Ig i.m soon following operation to Rh –ve mothers
OTHER TYPES OF ECTOPIC PREGNANCY
Ovarian and abdominal pregnancies occur rarely. The clinical picture of an ovarian pregnancy is similar to that of the tubal pregnancy. Abdominal pregnancy usually does not continue for considerable periods of time, but still cases have been repeated on full-term abdominal pregnancy. The fetus inside the membranes, grows in the space between the internal organs, the placenta being attached to the tube, the peritoneum or the inner organs. The pregnancy is pathological and the fetus would normally die. The dead fetus macerates and undergoes aseptic disintegration or mummification. Cases have been reported in which the dead fetus was macerated and necrotized due to entrance of infection from the intestine. Considerable intra-abdominal hemorrhage may occur in connection with separation of placenta. Ovarian and abdominal pregnancies are treated surgically.