Hepatocellular Carcinoma or Liver Cancer
Hepatocellular Carcinoma Or Liver Cancer: Causes, Clinal Features, Diagnosis and Management
• Hepatocellular carcinoma (HCC) is a primary malignancy of the hepatocyte, generally leading to death within 6-20 months.
• Hepatocellular carcinoma frequently arises in the setting of cirrhosis, appearing 20-30 years following the initial insult to the liver.
• 25% of patients have no history or risk factors for the development of cirrhosis.
• currently one of the most common worldwide causes of cancer death

Epidemiology: worldwide (China, sub-Saharan Africa, Japan)
Pathophysiology
• Tumors are multifocal within the liver 75% of the time. Late in the disease, metastases may develop in the lung, portal vein, periportal nodes, bone, or brain.
Mortality/Morbidity
- Cure, usually through surgery, is possible in fewer than 5% of all patients.
- Median survival from time of diagnosis is generally 6 months.
- portal vein occlusion, which occurs commonly,portends an even shorter survival.
- Complications from hepatocellular carcinoma are those of hepatic failure; death occurs from cachexia, variceal bleeding, or (rarely) tumor rupture and bleeding into the peritoneum
Race • Hepatocellular carcinoma is most commonly found among Asian persons, due to childhood infections with hepatitis B.
Sex
• Hepatocellular carcinoma occurs more commonly in men than in women
Age
• Hepatocellular carcinoma is rarely diagnosed in persons younger than 40 years.
• In Africa and Asia, age at diagnosis is substantially younger, occurring in the fourth and fifth decades of life, respectively.
Etiology
1. Cirrhosis
About 80% of patients with newly diagnosed hepatocellular carcinoma have preexisting cirrhosis attributed to alcohol, hepatitis C infection, and hepatitis B infection.
2.Hepatitis B virus
• Global incidence of chronic HBV infection is estimated to be 350 million persons; chronic HBV infection is the most common cause of hepatocellular carcinoma worldwide.
• Chronic infection in the setting of cirrhosis increases the risk of hepatocellular carcinoma 1000-fold.
3.Hepatitis C virus
• HCV is a global pandemic affecting 170 million persons. HCV infection results in a higher rate of chronic infection compared to HBV infection (approximately 80% of
infected subjects).
• It has become the most common cause of hepatocellular carcinoma in Japan and Europe. About 30% progress to cirrhosis, and in these, about 1-2% per year develop
hepatocellular carcinoma.
• Co-infection with HBV further increases the risk
4. Hemochromatosis:.
5. Aflatoxin: This hepatic carcinogen is a byproduct of fungal contamination of foodstuffs in sub-Saharan Africa and East and Southeast Asia. It causes DNA damage and mutations of the p53
gene.
Rare associations:
1. Primary Biliary Cirrhosis
2. Androgenic steroids,
3. Primary Sclerosing Cholangitis
4. 1-antitrypsin deficiency
5. Thorotrast radioactive contrast
6. Oral contraceptives
7. Porphyria cutanea tarda.
8. Obesity and diabetes have been implicated as risk factors for hepatocellular carcinoma ( related to NASH and Non Alcoholic Fatty Liver)
Clinical History
• Patients generally present with symptoms of advancing cirrhosis.
• Pruritis
• Jaundice
• Splenomegaly
• Variceal bleeding
• Cachexia
• Increasing abdominal girth (portal vein occlusion by thrombus with rapid development of ascites)
• Hepatic Encephalopathy
• Right upper quadrant pain (uncommon)Physical
• Jaundice
• Ascites
• Hepatomegaly
• Alcoholic stigmata (Dupuytren contracture, spider angiomata)
• Asterixis
• Pedal edema
• Periumbilical collateral veins
• Enlarged hemorrhoidal veins
Differential Diagnoses
A. Cholangiocarcinoma
B. Cirrhosis
C. Hepatocellular Adenoma
Other Problems to Be Considered
1. Dysplastic nodules in cirrhosis
2. Fibrous nodular hyperplasia
3. Metastatic disease
4. Primary hepatic lymphomaDiagnosis
Laboratory Studies
• Expect total bilirubin, aspartate aminotransferase (AST), alkaline phosphatase, albumin, and prothrombin time to show results consistent with cirrhosis.
• Alpha-fetoprotein (AFP) is elevated in 75% of cases.
• The level of elevation correlates inversely with prognosis.
• An elevation of greater than 400 ng/mL predicts for hepatocellular carcinoma with specificity greater than 95%.
• Alpha-fetoprotein (AFP) is inadequate for screening purposes because of the high rate of false positives in active hepatitis; it only begins to rise when vascular invasion occurs
Imaging Studies
- Ultrasonography
- An advantage is that Doppler imaging can be performed at the same time to determine the patency of the portal vein.
- CT scanning -Triphasic technique (ie, without contrast, then with early [arterial] and late [portal] imaging).CT scanning has the added benefit of detecting extrahepatic disease, especially lymphadenopathy.
- MRI-detect smaller lesions and can also be used to determine flow in the portal vein. The overall sensitivity of MRI is thought to be similar to that of triphasic CT scanning.
- Angiography-Shows characteristic tumor blush in hepatocellular carcinoma
- Chest radiography may demonstrate pulmonary metastases
- Bone scanning and head CT scanning are of low yield in the absence of specific symptoms.
- PET scan: Under experiment
- Biopsy-Frequently necessary for diagnosis.Core biopsy is favored over fine needle biopsy since larger amounts of tissue, often with normal surrounding parenchyma, can be obtained.
Biopsy may be omitted in a clinical setting of a growing mass in a cirrhotic liver (>2 cm) noted on 2 coincident imaging techniques with at least one imaging showing contrast enhancement.
Likewise, a growing mass in a cirrhotic liver on one imaging modality with an associated AFP level greater than 500-1000 ng/mL is clinically diagnostic of hepatocellular carcinoma . Biopsy is generally obtained percutaneously under ultrasonographic or CT guidance.
Using laparoscopic guidance may make obtaining a percutaneous biopsy easier. Obtaining a biopsy may be unnecessary in patients who will undergo resection regardless of diagnosis.
• One system is the CLIP (Cancer of the Liver Italian Program) scoring system, which assigns a cumulative prognostic score ranging from 0-6 based upon
1. Child-Pugh stage,
2. tumor morphology,
3. alpha-fetoprotein level,
4. and portal vein thrombosis,
5. can predict median survivalTNM staging criteria for hepatocellular carcinoma
• T1 – Solitary tumor without vascular invasion
• T2 – Solitary tumor with vascular invasion or multiple tumors none more than 5 cm
• T3 – Multiple tumors more than 5 cm or tumor involving a major branch of the portal or hepatic vein(s)
• T4 – Tumor(s) with direct invasion of adjacent organs other than the gallbladder or with perforation of visceral peritoneum
• N0 – Indicates no nodal involvement
• N1 – Indicates regional nodal involvement
• M0 – Indicates no distant metastasis
• M1 – Indicates metastasis presence beyond the liverStage grouping
• Stage I = T1 + N0 + M0
• Stage II = T2 + N0 + M0
• Stage IIIA = T3 + N0 + M0
• Stage IIIB = T4 + N0 + M0
• Stage IIIC = TX + N1 + M0
• Stage IVB = TX + NX + M1CLIP scoring system: Score of 0-2 is assigned for each of the 4 features listed below; cumulative score ranging from 0-6 is the CLIP score.
Child-Pugh stage Stage A = 0 Stage B = 1 Stage C = 2
Tumor morphology
Uninodular and extension less than 50% = 0
Multinodular and extension less than 50% = 1
Massive and extension greater than 50% = 2
Alpha-fetoprotein Less than 400 = 0, Greater than 400 = 1
Portal vein thrombosis Absent = 0 Present = 1
:Estimated survival based on CLIP score
• score of 0 – about 31 months;
• score of 1- about 27 months;
• score of 2- about 13 months;
• score of 3- 8 months;
• scores 4-6-approximately 2 months.Medical Care
Treatment:
1.Available treatment options depend on the size, number, and location of tumors; presence or absence of cirrhosis; operative risk based on extent of cirrhosis and comorbid diseases; overall performance status; patency of portal vein; and presence of metastatic disease.
2.Before instituting definitive therapy
• treat the complications of cirrhosis with diuretics,
• paracentesis for ascites, l
• actulose for encephalopathy,
• ursodiol for pruritus,
• sclerosis or banding for variceal bleeding, and
• antibiotics for spontaneous bacterial peritonitis.
• Surgical resection and liver transplantation are the only chances of cure but have limited applicability. Other local therapies are chemoembolization, ethanol ablation, radiofrequency ablation, cryoablation, and radiotherapy. Patients whose disease is downstaged following chemoembolization may be eligible for transplantation. Systemic treatment with chemotherapy may be used for advanced disease.
Systemic chemotherapy
The most active single agent drugs tested have been
• doxorubicin,
• cisplatin, and
• fluorouracil.
• Response rates are about 10%, and treatment shows no clear impact on overall survival.
• More recently, gemcitabine and capecitabine have been evaluated in clinical trialscisplatin-based combination regimens, such as gemcitabine and oxaliplatin, have shown improved response rates around 20%,
Chemoimmunotherapy uses a combination of chemotherapy and immunomodulatory agents,
- • such as interferon-alpha.
- • Antiangiogenesis agents (ie,bevacizumab), which work by disrupting the formation of blood vessels that feed tumors, are a new class of drugs that may prove to be of benefit in the treatment of hepatocellular carcinoma.
- • Sorafenib, a multitargeted oral kinase inhibitor, has recently been shown in a phase III trial to prolong survival in patients with hepatocellular carcinoma.
- Sunitinib
Erlotinib
• Embolizing agents such as cellulose, microspheres, lipoidal, and gelatin foam particles are used to deliver intra-arterial chemotherapy (mitomycin, doxorubicin, cisplatin) to the tumor via the hepatic artery.
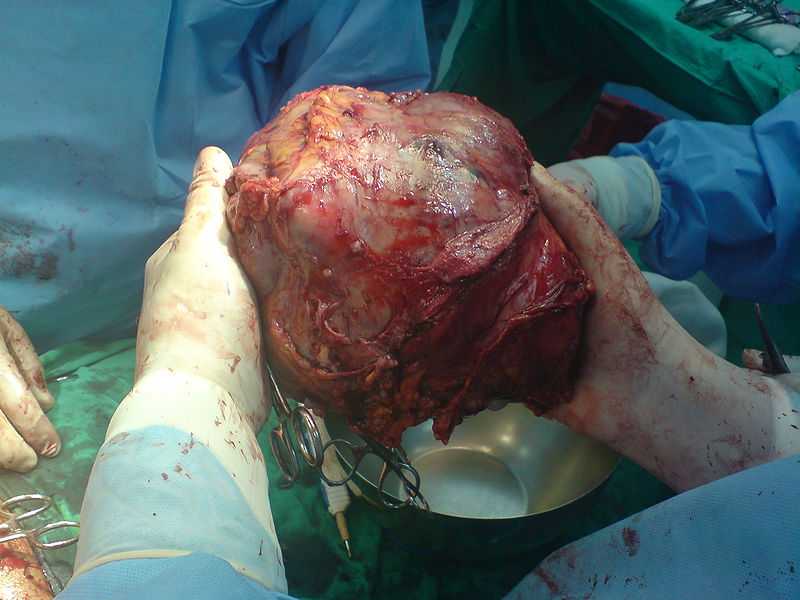
• Partial hepatectomy
• Orthotopic liver transplantation can be considered for patients.
• Local tumor ablation
• Intratumoral injections of ethanol or acetic acid, heat (via radiofrequency, microwave, or laser
ablation), or cold (cryoablation with liquid nitrogen) may be used to locally control tumors smaller
than 4-5 cm. These techniques are frequently performed percutaneously as outpatient
procedures. In general, these procedures are reserved for patients who do not meet criteria for
surgical resection yet are candidates for a liver-directed procedure based on the presence of
limited liver-only disease.
• Radiofrequency ablation (RFA) is the delivery of radiofrequency thermal energy to the
hepatocellular carcinoma lesion causing necrosis of the tumor.
• Percutaneous ethanol or acetic acid ablation is reserved for patients with small tumors; however,
in many areas, the ease and efficacy of RFA has now replaced these older techniques.
Radiation therapy is limited by dose-related radiation hepatitis, which precludes the
administration of external beam radiation in doses effective for tumor eradication. Doses of 2500
cGy may be used for palliative measures.
• CyberKnife system is a new technology that uses a combination of robotics and image guidance
to deliver concentrated and highly focused beams of radiation to the tumor while minimizing
radiation exposure to the surrounding healthy liver tissue.
Summarized- Source Medscape.com, Bailey and Love’s manual of surgery, wikipedia, Manipal book of Surgery




1 Comment
Very good article, but some statements more difficult to understand, the proposed wiki plug-ins for these clauses,Make the article more easy to understand!
Comments are closed.