Myocardial Infarction Made Easy
The 4 Ischemic Heart Diseases caused due to imbalance between supply and demand of the heart for oxygenated blood are:
- Acute Myocardial Infarction (MI)
- Angina Pectoris
- Chronic Ischemic Heart Disease (IHD)
- Sudden Cardiac Death
Myocardial Infarction (MI) Commonly known as a heart attack, is an anemic infarct with coagulative necrosis of a large area of the myocardium due to occlusion of one of the three main trunks of the coronary arteries.
Types:
| Basis of Difference | Transmural Infarct | Subendocardial Infarct |
| Definition | Full-thickness, solid | Inner 1/3rd to 1/2nd, patchy (mosaic infarct) |
| Frequency | More frequent (95%) | Less frequent |
| Distribution | Specific area of coronary supply | Circumferential |
| Pathogenesis | Absolute persisten ischemia as a result of stenosis of one main trunk of coronary artery | Worsening of temporary relative ischemia as a result of stenosis of one or more main trunk of coronary arteries |
| Coronary thrmobosis | Common | Rare |
Risk Factors:
- Age: Increased
- Sex: Male
- Other Predisposing factors of atherosclerosis (Predisposing factors and Pathogenesis of Atherosclerosis)
Pathogenesis:
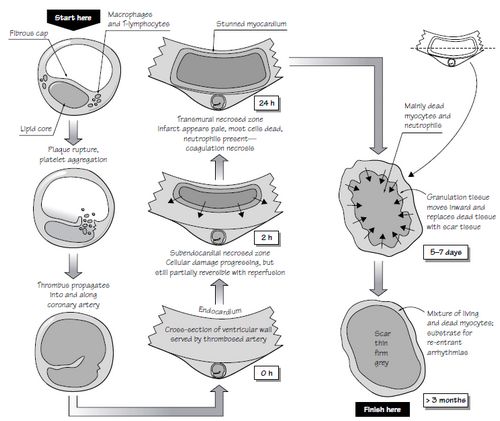
A) Coronary Artery Occlusion:
Mechanisms:
1. Coronary Atherosclerosis:
Distribution: Left Anterior Descending (LAD) CA> Right Coronary Artery (RCA)> Left Circumflex (LCX) CA
Process:
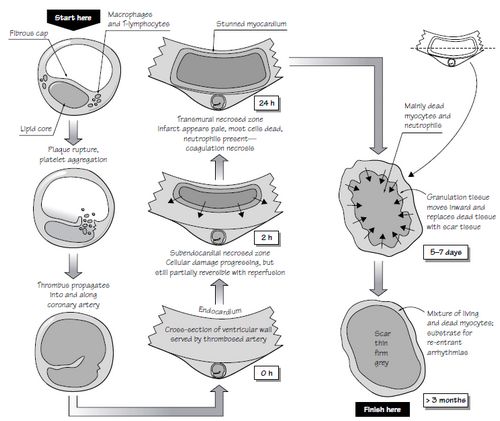
- Atherosclerotic Plaque Disruption (rupture/fissuring, erosion/ulceration, hemorrhage i.e. complicated atherosclerosis) leading to exposure of subendothelial collagen and necrosis of plaque. Plaques having more foam cells, extracellular lipid, inflammatory cells, less smooth muscle cells and thin fibrous cap are the vulnerable plaques. Activated macrophages and T-lymphocytes localized at the site of plaque rupture are thought to release metalloproteases and cytokines which weaken the fibrous cap.
- Sequence of process of hemostasis:
- Adhesion, aggregation and activation of platelets and release of aggregators including TXA2 (Thromboxane A2), serotonin, etc.
- Vasospasm
- Extrinsic pathway of coagulation cascade activated to form thrombus
- Complete occlusion of coronary vessel lumen
2. Non-atherosclerotic Vasospasm
3. Emboli: Left sided mural thrombus, Endocarditis, Paradoxical emboli
4. Unexplained: Amyloid, Hemoglobinopathies
B) Myocardial Response:
- Loss of critical blood supply to myocardium
- Decreased aerobic glycolysis and Increased anaerobic glycolysis
- Decreased ATP and Increased Lactate accumulation
- Loss of contractility
- Acute Heart Failure
- Microvascular injury leading to Coagulative necrosis
| Feature | Time |
| Onset of ATP depletion | Seconds |
| Loss of contractility | < 2 min |
ATP Depletion
|
10 min 40 min |
| Irreversible cell injury | 20-40 min |
| Microvascular injury | >1 hour |
Morphology
1. Anterior wall infarcts: Occlusion of Left Anterior Descending (LAD) Coronary artery
2. Posterior wall infarcts: Occlusion of Right Coronary artery
3. Lateral wall infarcts: Occlusion of Left Circumflex (LCX) Coronary artery
Gross Features by Time from Onset:
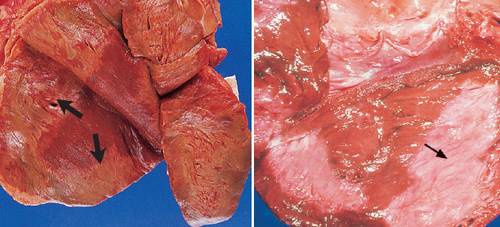
Acute Infarction: Pale infarction with cyanotic areas of hemorrhages and yellow border (Correlate with Microscopic changes of Coagulative necrosis and Acute inflammatory changes)
- 12-24 hours: Pallor
- 24-72 hours: Pallor, sometimes hyperemia; yellowing at periphery (due to neutrophilic infiltration)
Subacute Infarction: Central yellow softening with hyperemic border (Correlate with Microscopic features of phagocytosis and healing)
- 3-7 days: Hyperemic border; central yellow-brown softening
- 1-3 weeks: Maximally yellow and soft with depressed red-brown hyperemic margins (due to growth of granulation tissue)
Old Infarction: Fibrosis
- 6 weeks: Mature Grey white fibrous scar and compensatory hypertrophy of the rest of the myocardium
Microscopic features by Time from Onset:
Acute Infarction: Caogulative necrosis with loss of striations and Acute Inflammatory reaction
- 1/2 to 4 hours: Waviness of fibers at border
- 4-12 hours: Beginning coagulation necrosis; edema; focal hemorrhage, beginning neutrophilic infiltration
- 12-24 hours: Continuing coagulation necrosis with loss of cross striations; pyknotic nucleus; myocyte contraction bands
- 1 -3 days: Coagulation necrosis completes with loss of nucleus and striations; neutrophilic infiltrate
Subacute: Appearance of macrophages, phagocytosis and Healing reaction
- 3-7 days: Disintegration of myofibers and phagocytosis by macrophages
- 1-3 weeks: Completion of phagocytosis; prominent granulation tissue with neuvascularization and fibrovascular reaction
Old: Fibrosis
- 6 weeks: Mature fibrous scar
Electron microscopy:
- Reversible phase (0-1/2 hours): Glycogen depeltion; mitochondrial swelling and relaxation of myofibrils
- Irreversible phase (>1/2 hours): Sarcolemmal disruption, Mitochondrial amorphous densities
Reperfusion Injury:
Reperfusion after ischemia overloads the tissue surrounding the necrotic area with calcium. This produces a continuous spasm leading to necrosis with contraction bands.
Complications:
- Arrhythmias and Conduction defects with possible sudden cardiac death
- Cardiogenic shock
- Mural thrombosis with possible embolization
- Myocardial rupture leading to cardiac tamponade and arrest
- Infarct extension or re-infarction
- Fibrinous pericarditis
- Papillary muscle necrosis with possible valvular insufficiency
- Congestive Heart Failure
- Myocardial aneurysm resulting from ventricular akinesis
Mnemonic: HEART PASs away during MI
- H: Heart Failure
- E: Embolism following Mural thrombus formation
- A: Arrhythmia which may lead to Sudden cardiac death
- R: Re-infarction
- T: Tamponade following Myocardial rupture
- P: Pericarditis and Dressler’s syndrome; Papillary muscle necrosis
- A: Aneurysm (Ventricular) resulting from Akinesis
- Ss: Shock (Cardiogenic)
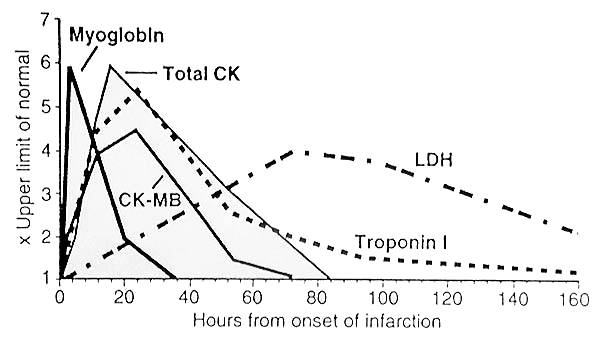
Cardiac markers:
Clinical Features, Diagnosis and Treatment of Myocardial Infarction