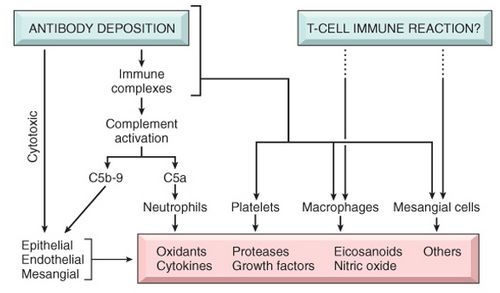
Pathogenesis of Glomerular Injury
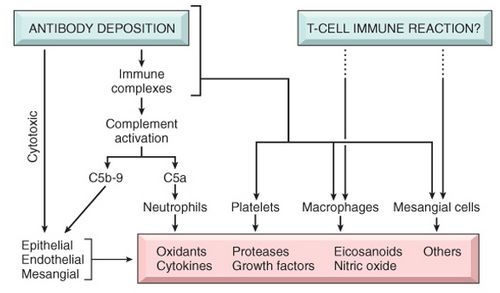
Primary Immunopathogenic mechanism:
Initiator of the disease process by:
- Antibody mediated injury: immune complex deposition or cytotoxic antibodies
- T-cell mediated immune injury: non-immune complex deposition mechanism
Secondary immunopathogenic mechanism:
Role of mediators of the disease:
A) Cells:
- Neutrophils and monocytes
- Macrophages, T lymphocytes and NK cells
- Platelets
- Resident glomerular cells (Mesagnial cells)
B) Soluble mediators:
- Complement components
- Eicosanoids, NO, angiotensin and endothelin
- Cytokines: IL-1 and TNF
- Chemokines: MCP-1, RANTES, TGF-B
- Coagulation system
Antibody Mediated Injury
Include:
- Membranous glomerulonephritis
- IgA nephropathy
- Membranoproliferative glomerulonephritis
- Postinfectious glomerulonephritis
- Anti-glomerular basement membrane disease
Immune complexes activates complement pathway through classic pathway.
A) In-situ immune complex deposition
1. Fixed intrinsic tissue (Glomerular) antigens:
Mechanism: Circulating antibodies form immune complex against the normal glomerular components
- Glomerular basement mebrane antigens : NC1 domain of collagen type IV antigen (anti-GBM disease)
- Immunofluorescence: Linear pattern immune-complex deposition
- Podocyte antigens: Heymann antigen (membranous glomerulonephritis)
- Immunofluorescence: Granular pattern immune-complex deposition
- Mesangial antigens
- Others
2. Planted (Deposited) antigens
Mechanisms: Non-glomerular antigens are deposited in GBM from the circulation firstly and then the circulating antibodies form immune-complex.
Immunofluorescence: Granular pattern immune-complex deposition
- Exogenous antigens (infectious agents, drugs)
- Endogenous antigens (DNA, nuclear proteins, immunoglobulins, immune complexes, IgA)
Factors influencing antigen trapping are: size, charge, molecular configuration and carbohydrate content of antigens.
B) Circulating immune complex deposition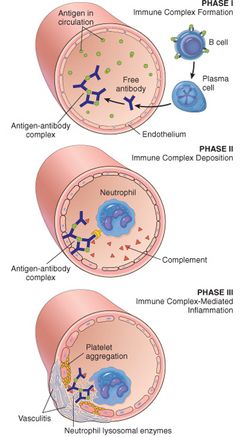
Immunofluorescence: Granular pattern immune-complex deposition
Mechanism: Type III hypersensitivity initiated by antigen-antibody complex formed in the circulation.
- Exogenous antigens (infectious products)
- Endogenous antigens (DNA, tumor antigens)
Localisation of complexes and Factors enhancing it:
Primary immune complex deposition in one site is often accompanied by deposition of lesser amounts in other sites. The factors influencing the localisation complexes are: molecular charge of complexes, size, avidity (strength of bond between antigen and antibody), blood flow, etc.
1. Subendothelial (between capillary endothelium and GBM):
- Charge: Highly anionic complexes excluded from GBM
- Size: Intermediate
- Avidity: High
2. Intramembranous (within GBM):
- Charge: Represents the transitional phase in which complexes migrate from subendothelial position to subepithelial
- Blood flow: Increased
3. Subepithelial (between epithelial cells and GBM):
- Charge: Highly cationic complexes
- Size: Smallest (pass freely through the glomerulus without being trapped)
- Avidity: Low
4. Mesangial (within mesangium):
- Charge: Neutral charge
- Size: Large
- Blood flow: Decreased
C) Cytotoxic antibodies
Cell mediated immune injury
Mechanism: Non-immune complex deposition glomerulonephritis
This may occur through regulation of B-cell differentiation and antibody production or by local cell-mediated immunity i.e. delayed-type hypersensitivity reaction. The later is initiated by CD4+ cells by activating monocytes/macrophages which produces cytokines: IL12, IL2, INF-γ and TNF-a which are powerful inflammatory mediators causing injury. CD8+ cells acts by their cytotoxic ability.
Includes:
- Minimal Change Disease (Lipoid necrosis)
- Focal segmental glomerulosclerosis
Activation of Alternative Complement Pathway
Alternative pathway of complement pathway is activated by complex polysaccharides.
Role of Complement: C3 & C5 are chemoattractant for leukocytes, neutrophils in particular which causes damage by releasing proteolytic enzymes and by generating reactive oxygen metabolites. Terminal complement components C5b-9, membrane attack complex (MAC) causes injury by basement membrane lysis.
Non-immunologic Mechanism
Hemodynamic and physical forces that cause intraglomerular HTN and abnormal stress and strain on the vascular wall.
Relationship of Physiologic role of glomerular components with consequences of glomerular injury
A) Endothelial cells:
Physiologic function –> Consequence of injury –> Related Disease
- Maintain glomerular perfusion –> Vasoconstriction –> Acute renal failure
- Prevent leukocyte adhesion –> Leukocyte infiltration –> Focal/diffuse GN
- Prevent platelet aggregation –> Intravascular microthrombi –> Thrombotic microangiopathies
B) Mesangial cells:
- Physiologic function: Control glomerular filtration
- Consequence of injury: Proliferation and increased matrix
- Related Disease: Membranoproliferative GN
C) Visceral epithelial cells (Podocytes):
- Physiologic function: Prevent plasma protein filtration
- Consequence of injury: Proteinuria
- Related disease: Minimal change disease, Focal Segemntal Glomerulosclerosis
D) Glomerular Basement Membrane (GBM):
- Physiologic function: Prevents plasma protein filtration
- Consequence of injury: Proteinuria
- Related disease: Membranous GN
E) Parietal epithelial cells:
- Physiologic function: Maintain Bowman’s space
- Consequence of injury: Crescent formation
- Related disease: Rapidly Progressive Glomerulonephritis (RPGN)
Summary:
a) Non-immune mechanisms are involved in Diabetic nephropathy
b) Detected anibody deposition pattern: Granular except in Anti-GBM Nephritis (Linear)
c) Sites of Immune complex or Antigen Deposition:
- Subepithelial: Poststreptococcal Glomerulonephritis
- Epimembranous: Membranous Glomerulonephritis
- Subendothelial: SLE, Type I Membranoproliferative Glomerulonephritis (MPGN)
- Mesangial: IgA Nephropathy
- Basement membrane: Type II MPGN